Original Research Article - (2022) Volume 12, Issue 1
We report an unusual finding of tumor involving the ulnar nerve in the hand. An 18-year-old female patient presented with a soft swelling in her right hand for 10 years. Neurological examination was normal. However, she had discomfort or pain when using her right hand frequently. Surgical exploration revealed that ulnar nerve and its digital branches were infiltrated by fibrolipomatous tissues. The infiltrating tumor underwent surgical debunking as it was encircling the ulnar nerve. Histological examination yielded the diagnosis of a neural fibrolipoma of the ulnar nerve. The result of surgical debulking was satisfactory. Postoperatively, there was no neurologic deficit and the patient had normal sensation and motor function.
Neural fibrolipoma • Ulnar nerve • Lipofibromatous hamartoma
Neural fibrolipoma is a localized, benign, slowly growing fibrofatty tissues around major nerves and their branches. Lipofibromatous hamartoma is an unusual tumor-like lesion that most commonly involves the median nerve or its branches [1-5]. However, involvements of the ulnar nerve, radial nerve, superficial peroneal nerve and brachial plexus have been [6-9] rarely reported in the literature. Usually, this tumor is painless and the patient’s main complaint is either the swelling itself or discomfort when using the hand throughout the day. Soft tissue masses in the hand encompass a wide list of many lesions, and lipofibromatous hamartoma should be on that list. We present in this report, an 18-year-old female patient with lipofibromatous hamartoma involving the ulnar nerve of right hand and its surgical management.
History
An 18- year-old female patient, who is medically free, right-handed, presented with right hand swelling (in her palm) that had been present for ten years.
The swelling was increasing gradually and slowly in size with time, associated with mild discomfort or pain whenever she used her right hand frequently. There was no reported history of discharge or bleeding from the mass. The patient did not have any numbness or tingling in her right hand. There was no weakness in her grip power. She did not have any prior history of trauma to her right hand. There were no other similar swellings in her body. Her family history was unremarkable. No history of smoking and no drug or food allergies.
Physical examination
The patient was conscious, alert and oriented. Her vital signs were within normal. Concerning her right hand, there was a swelling in the palm area mainly on the ulnar most aspect that was oriented longitudinally between the 5th and 4th rays (Figure 1). The size of the swelling was (3 × 7) cm. It had a smooth surface with ill-defined edges. There were no bruit or thrills. The swelling was not compressible. The overlying skin had normal color. Capillary refill in all digits were less than 2 seconds. Allen’s test showed intact palmar arch. The patient was able to make a full fist with her right hand. She had absent Tinel’s sign over the swelling. Her neurological examination of right hand was within normal.

Figure 1: Showing swelling in the ulnar aspect of the palm.
Investigations
Her preoperative lab results were within normal limits.
MRI: MRI examination of her right hand showed; there is a well-defined superficial lesion in the right medial aspect of the pattern between the 4th and the 5th metacarpal rays measuring (1.1 × 1.6 × 3.4) cm lesion which shows heterogenous high signal intensity on T-1 with loss of signal in the T-1 fat sat in keeping with a fat containing lesion. There is no abnormal enhancement post contrast, no invasion into the adjacent tendons. Normal signal intensity of the bone. No erosions, fractures, or dislocations. Normal signal intensity of the extensor and flexor compartments. Normal joint spaces.
Impression: Right palmar lesion between the 4th and the 5th metacarpal rays noted of the flexor zone III extended into flexor zone II as described in keeping with lipoma (Figures 2-4).
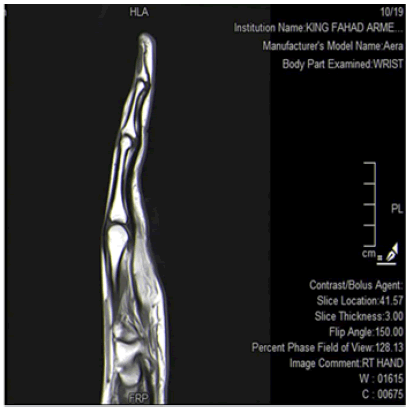
Figure 2: Showing superficial soft tissue swelling in the palm.
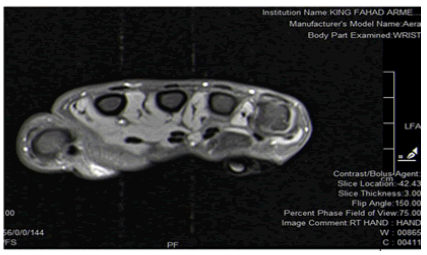
Figure 3: Showing superficial soft tissue swelling in the palm; between 4th and 5th metacarpal rays.
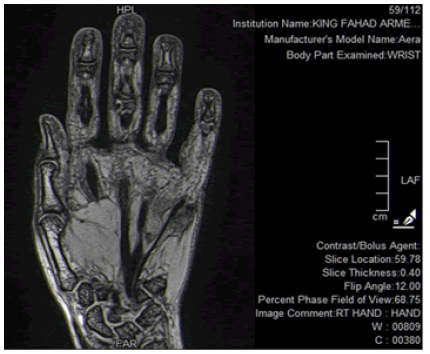
Figure 4: Showing superficial soft tissue swelling in the palm; between 4th and 5th metacarpal rays.
Ultrasound: Showed a well-defined hyperechoic area with no increased interval vascularity measuring (5.2 × 1) cm.
Most likely representing a lipoma vs other pathology (Figure 5).
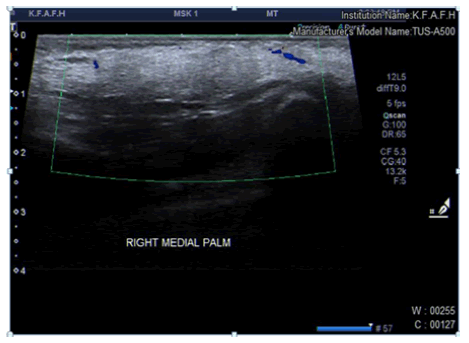
Figure 5: Showing superficial soft tissue swelling in the palm.
Procedure
After thorough discussion with the patient and her parents, counseling regarding the possible nature of the swelling and the procedure risks versus benefits, she was elected to undergo excisional biopsy of that swelling in her right palm under general anesthesia as a day surgery procedure. We decided to approach the swelling through Bruner type incision (zig-zag), using 15- blade (Figure 1). Following the elevation of skin flaps, subcutaneous tissue dissection was carried out using tenotomy scissor until we reached the site of the swelling. It was evident intraoperatively, that this swelling had a fusiform character and with fibrofatty texture. It was found along the distribution of ulnar nerve distal to Guyon’s canal (Figure 6). This fibrofatty tumor was encircling the superficial sensory branch of ulnar nerve only, but without any involvement to the deep motor branch. It was clear that this nerve had undergone hypertrophy throughout its course. Therefore, the decision to completely resect this tumor without injuring the superficial sensory branch of ulnar nerve was not possible. If we had to resect the entire tumor then we would have to sacrifice the superficial sensory branch distal to zone III of Guyon’s canal and with a resulting gap of 7 cm. Thus, we proceeded towards precise microvascular tumor debulking as much as possible using 3.5x loupe magnification and microinstruments (Figure 7). After achieving satisfactory tumor debulking, it was again noticeable to us that the involved nerve was thickened and hypertrophied. However, there was no iatrogenic injury to the ulnar nerve. The specimen was sent to histopathology lab for definitive diagnosis. The procedure was uneventful and the patient was discharged home on the same day in stable condition.
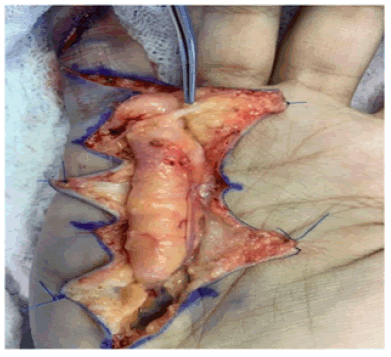
Figure 6: Intraoperative view of the tumor encircling the ulnar nerve.

Figure 7: After surgical debulking of the tumor off the ulnar nerve.
Histopathology
Right hand mass: Consistent with Fibrolipoma. Negative for atypia and malignancy.
Follow-up
Her first postop visit to the clinic was one week postop. The patient did not report any sensory deficits or any problems with regards to her motor function. She was satisfied with the debulking done. The patient was referred to our occupational therapist for range of motion exercises and scar management. Sutures were removed in the 2nd visit which was two weeks postop.
Neural fibrolipoma (neurolipomatosis, lipofibromatous hamartoma of nerves, and macrodystrophia lipomatosa) is a rare, slow-growing tumor consisting of proliferating fibrofatty tissue surrounding and infiltrating major nerves and their branches [1]. The etiology in most cases is unknown although some cases may be associated with previous history of trauma to the hand. Neural fibrolipomas are most often seen during the first 3 decades of life and may sometimes be considered as congenital lesions. Of 26 cases reported by Silverman and Enzinger [2], there were no patients older than 40 years of age. The median nerve is most often affected, but involvement of the ulnar, radial, peroneal, and cranial nerves and brachial plexus has been described in the literature. The usual symptoms of neural fibrolipoma are pain, an enlarging mass and diminished sensation. Macrodactyly occurs in approximately one third of patients [2].
This lesion was described with different names such as “neurolipomatosis”, “neural fibrolipoma” and “macrodystrophia lipomatosa” [7]. Bibbo and Warren reported that upper extremity cases would typically present before the age of 25, usually without macrodactyly and without a documented history of trauma [7]. Neural fibrolipoma is characterized histologically by fibrofatty tissue that surrounds and infiltrates the nerve, and it may cause thickening of the perineurium and perivascular fibrous tissues [3]. The perineurium shows concentric thickening with pseudo-onion bulb-like change. Rare cases show foci of metaplastic bone [1]. Complete excision of the fibrofatty growth is contraindicated because it may cause severe sensory or motor disturbances [8]. If necessary, biopsy of a small cutaneous nerve can establish the diagnosis [1]. Other treatment recommendations include decompression of the carpal tunnel, microsurgical intraneural dissection of neoplastic elements, and excision of the involved nerve with or without nerve grafting [4,10]. Pain relief can be obtained with surgical debulking of the involved nerve [4]. Because neural fibrolipoma presents as a deep-seated mass, conventional punch biopsy may not disclose the proper diagnosis [4], and surgical exploration may be needed.
Surgical debulking is a satisfactory treatment option when it comes with dealing with lipofibromatous hamartoma that is infiltrating and encircling a major nerve. The aim of surgical debulking is to avoid any sensory or motor deficit from iatrogenic injury that could ensure during the resection process. This tumor although rare it should be thought of in the working diagnosis of patients with soft tissue tumor of the hand.
Citation: Alkabbaa S, Felimban M (2022) The First Reported Case of Neural Fibrolipoma of Ulnar Nerve in the Hand in Saudi Arabiar, Surg Curr Res 12(1), 369.
Received: 30-Dec-2021, Manuscript No. SCR-21-14416; Editor assigned: 03-Jan-2022, Pre QC No. SCR-21-14416; Reviewed: 17-Jan-2022, QC No. SCR-21-14416; Revised: 18-Jan-2022, Manuscript No. SCR-21-14416; Published: 24-Jan-2022, DOI: 10.35248/2161-1076.22.12.1.369
Copyright: ©2021 Alkabbaa S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.