Case Report - (2024) Volume 9, Issue 1
Cutaneous Tuberculosis (TB), primarily caused by Mycobacterium tuberculosis, is a rare and clinically polymorphic disease, making diagnosis challenging. Diagnosis relies on epidemiological, clinical, and para-clinical evidence. Treatment with TB antibiotics typically yields excellent results, often retrospectively confirming the diagnosis. We report a case of scrofuloderma in a 33-year-old woman presenting with a painful, purulent nodule on her inter-scapular area. Initial misdiagnosis as a bacterial abscess delayed effective treatment. Following a confirmed diagnosis of scrofuloderma, anti-TB therapy led to significant clinical improvement, underscoring the importance of considering TB in persistent cutaneous lesions.
Cutaneous tuberculosis • Mycobacterium tuberculosis • Scrofuloderma • Anti-TB therapy
Cutaneous tuberculosis (TB), caused primarily by Mycobacterium tuberculosis, is a rare and often perplexing manifestation of TB, accounting for only 1%-2% of extrapulmonary TB cases [1]. Its rarity and clinical polymorphism make diagnosis challenging. The diagnostic process relies heavily on a combination of epidemiological data, clinical presentation, and para-clinical evidence. Despite these challenges, the prognosis for cutaneous TB is generally excellent with appropriate treatment using TB antibiotics. Retrospective confirmation of the diagnosis is often achieved through the patient's positive response to therapy. In this article, we discuss a case of scrofuloderma in a 33-year-old woman, highlighting the diagnostic journey and successful treatment outcome [2].
We present a case of a 33 year old woman from the countryside of, she complained about a painful nodule on her inter-scapular area that started 7 months before, after a few months the lesion enlarged, became painful and oozing purulent secretions. She had been treated for bacterial abscess by several physicians with antibiotics analgesics without improvement. On physical examination the patient was afebrile, bilateral axillary and cervical lymph nodes were detected. Dermatologic examination revealed an excavated ulceration with a foul-smelling fluid oozing from the sore. The peri-ulcerated area was infiltrated and very sensitive to contact. The patient denied any systemic symptoms, she lived with her brother who was previously diagnosed with pulmonary tuberculosis [3,4].
Given the chronicity and characteristics of the lesion, as well as her brother’s history of pulmonary TB, scrofuloderma was suspected as the primary diagnosis. Blood examinations, including serologies for HIV and viral hepatitis, were normal, and chest radiography did not show abnormalities. However, the tuberculin skin test (IDR) was strongly positive (23 mm). A biopsy of the lesion revealed granulomas without caseating necrosis, and Ziehl-Neelsen staining did not demonstrate bacilli [5]. Despite the absence of definitive microbiological evidence, the clinical and epidemiological context strongly suggested cutaneous TB. The patient was started on a standard anti-TB regimen, resulting in significant improvement within a few weeks, thereby confirming the diagnosis retrospectively.

Figure 1: Excavated ulceration on the inter-scapular.
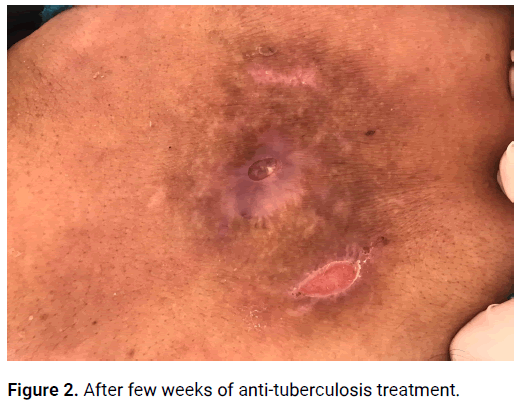
Figure 2: After few weeks of anti-tuberculosis treatment.
On physical examination, the patient was afebrile. However, bilateral axillary and cervical lymphadenopathy was noted. Dermatological examination revealed an excavated ulceration oozing foul-smelling fluid. The peri-ulcerative area was infiltrated and highly sensitive to touch. Despite these significant local symptoms, the patient denied any systemic manifestations of illness. A critical piece of her medical history was her living situation with a brother previously diagnosed with pulmonary TB.
This epidemiological context, combined with the lesion's clinical characteristics, led to a strong suspicion of scrofuloderma [6].
Cutaneous TB represents a minor fraction of TB cases but poses significant diagnostic challenges. The disease can manifest in various forms, including scrofuloderma, lupus vulgaris, tuberculous chancre, and tuberculosis verrucosa cutis, each presenting with different clinical features. Scrofuloderma, as seen in this case, results from the direct extension of TB from an underlying tuberculous lesion, often in lymph nodes or bones, to the skin [7].
The rarity of cutaneous TB and its diverse clinical manifestations often lead to misdiagnosis or delayed diagnosis. In our case, the patient was initially treated for a bacterial abscess, a common misdiagnosis due to the ulcerative nature of the lesion. The persistence of symptoms despite antibiotic treatment and the lack of systemic symptoms should prompt clinicians to consider alternative diagnoses, including cutaneous TB, especially in patients with relevant epidemiological exposures.
Diagnosis of cutaneous TB relies on a combination of clinical evaluation, histopathological examination, and microbiological tests. While histopathology typically reveals granulomatous inflammation, the absence of caseating necrosis and negative Ziehl-Neelsen staining does not rule out TB. A positive tuberculin skin test or Interferon-Gamma Release Assay (IGRA) supports the diagnosis, particularly in endemic areas or in patients with known TB contacts. Given the clinical presentation, epidemiological context, and diagnostic findings, a presumptive diagnosis of scrofuloderma was made. Scrofuloderma, a form of cutaneous TB, typically arises from the direct extension of Mycobacterium tuberculosis from an underlying tuberculous focus in lymph nodes or bone to the skin [8].
The patient was started on a standard anti-TB regimen, consisting of a combination of first-line TB antibiotics: isoniazid, rifampicin, pyrazinamide, and ethambutol. This regimen, typically administered over a period of six months, aims to eradicate the infection comprehensively. The patient's response to treatment was remarkable. Within a few weeks, there was significant improvement in the ulcerative lesion. The pain and purulent discharge diminished, and the ulcer began to heal. By the end of the treatment course, the lesion had healed completely, and there were no signs of recurrence. This excellent therapeutic response not only confirmed the diagnosis of scrofuloderma retrospectively but also underscored the effectiveness of TB antibiotics in treating cutaneous manifestations of the disease [9].
Cutaneous tuberculosis represents only 1%-2% of extrapulmonary forms of tuberculosis, scrofuloderma results from direct extension of the bacilli from an underlying tuberculous lesion in lymph nodes or bone. TB continues to be a major public health especially in third world countries, therefore all its clinical forms should be thoroughly known to physicians to enable an early diagnosis and an adequate treatment. This case exemplifies the importance of considering TB in differential diagnoses of chronic skin lesions and the pivotal role of TB antibiotics in achieving excellent therapeutic outcomes. Continued awareness and education among physicians regarding the varied manifestations of TB are vital in improving early diagnosis and treatment, thereby reducing the burden of this enduring public health challenge.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Belanouane S, et al. "Scrofuloderma: A Rare Case of Cutaneous Tuberculosis". J Dermatol Case Rep, 2024, 9(1), 1-2.
Received: 15-Jan-2024, Manuscript No. DMCR-24-4777; Editor assigned: 18-Jan-2024, Pre QC No. DMCR-24-4777 (PQ); Reviewed: 01-Feb-2024, QC No. DMCR-24-4777; Revised: 15-May-2024, Manuscript No. DMCR-24-4777 (R); Published: 12-Jun-2024, DOI: 10.37532/2684-124X.24.9.1.003
Copyright: © 2023 Belanouane S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.