Case Report - (2022) Volume 11, Issue 5
This clinical case reveals an example of the application of an iliac crest bone graft for the reconstruction of the metacarpal shaft defect, acquired as a result of a shrapnel injury.
Iliac crest bone graft • Metacarpal shaft defect • Shrapnel injury
Around 400 patients with shrapnel injuries were admitted to our Department of Plastic & Reconstructive Surgery and Microsurgery at the University Clinical Hospital after Mkhitar Heratsi, during the second war in the Nagorno-Karabakh region [1]. Most of the cases had severe soft tissue and bone defects, which demand specialized reconstructive approaches for appearance and functional restoration.
Predominantly, shrapnel injuries tend to develop soft-tissue and bone infections (e. g. gas gangrene, necrotizing fasciitis, osteomyelitis, etc.) [2]. All the aforementioned extend the post-operative healing course and provide unacceptable outcomes.
Reconstructive management of bone defects includes autologous grafts, allografts, and/or artificial materials [1-10]. In reconstructive surgery, the most applicable autologous grafts are iliac crest bone graft, fibular graft, and scapular graft [1-3]. The previously mentioned grafts can be used both as a graft with vascular pedicle and as a non-vascularized graft.
Historical reference
For the first time, anterior iliac crest bone grafting (AICBG) has been used during First World War by German surgeons Lindermann of Dusseldorf and Klapp of Berlin for oral & maxillofacial reconstruction. In Armenia, the reconstruction of a metacarpal bone defect with an iliac crest bone graft firstly was performed by Ph.D. Sahakyan A. B.
A 29-year-old police officer on 4th of October, 2020 was admitted to the Emergency Department of the University Clinical Hospital N1 after Mkhitar Heratsi with multiple shrapnel injuries in the region of the head, face, right shoulder, right and left hands, thorax, and both lower limbs. In the hospital, the patient was thoroughly examined and the X-ray radiographs demonstrate fractures of the right clavicle, multi-fragmentary fracture of the 2nd and 3rd metacarpal bones of the right hand, and the presence of metal splinter in the shaft of the 2nd metacarpal bone.
Under general anaesthesia, primary surgical treatment of wounds was performed by reconstructive micro surgeons, traumatologists, and maxillofacial surgeons. All the metal splinters were removed, including the splinter from the region of the 2nd metacarpal bone (approximately 2.5x2.0 cm) and as a result of the latter; a large bone defect was formed. Before the fixation of fragments of the 2nd and 3rd metacarpal bones, a wound swab test was done for anaerobic and aerobic infection detection and antibiotic sensitivity.
To prevent the movement of bone fragments, intra-operatively a decision has been made to stabilize them using Kirschner wires (K-wires). Fixations of the right shoulder joint were performed by traumatologists. The postoperative course was sufficient; the patient was prescribed a 2-week course of antibiotics [9]. In December 2020, the patient was once again admitted to the Department for Plastic & Reconstructive Surgery and Microsurgery for further reconstruction of the 2nd metacarpal bone (Figures 1 and 2). Considering the patient's previous injuries, surgeries, and general exhausted state, it was decided to use a non-vascularized anterior iliac crest bone graft.

Figure 1: Preoperative radiographs on both projection.

Figure 2: Preoperative radiographs.
Under general anaesthesia, a tourniquet was placed on the border of the lower and middle 1/3 of the forearm. Secondary surgical treatment of the wound was performed, the K-wires of the 2nd and 3rd metacarpal bones were removed and the existing bone defect of the 2nd metacarpal shaft was measured (nearly 4cm in length and 1cm in width). Secondary stabilization of the 3rd metacarpal bone was done, after bone fragment repositioning (Figures 3-5). Subsequently, a bicortical bone graft was harvested 3cm posterior to the anterior superior iliac spine (ASIS), using the subcostal-window technique.

Figure 3: Preoperative appearance of the right hand in operation table.

Figure 4: Defect of the metacarpal bone

Figure 5: Harvested Anterior Iliac Crest Bone Graft.
The outer and inner cortices of the iliac crest were fixed together with sutures (prolene4.0)(Figure 6).The harvested bone graft was repositioned so that it bridged the proximal and distal articular heads of the 2nd metacarpal bone and was secured with a single K-wire.

Figure 6: Harvested Anterior Iliac Crest Bone Graft
Radical debridement and primary reconstruction of the existing injury is the preferable option for each reconstructive surgeon. Regardless of the advantages of the mentioned sequence of procedures, e. g. reduction of postoperative morbidity, infection rate, decreased myriad of procedures, and hospital stay, they are not applicable for all types of injuries. In the described case, counting the type of trauma, accompanying injuries, the patient’s exhausted state, and high risk of infection was decided to postpone secondary reconstruction for 2 months.
The existent options for secondary reconstruction include both alloplastic and autogenic bone grafts. The prevailing alloplastic grafts are hydroxyapatite, calcium carbonate, and tricalcium phosphate [1]. The properties of alloplastic grafts largely meet the requirements necessary for bone regeneration; however, some components of these grafts can be completely resorbed in a short period. The latter was the main reason for abandoning this option, as long-term stabilization was needed in the presented case.
Autogenic bone grafts are always taken into account as first-choice options for such controversial cases. The commonly used donor areas for bone graft harvesting are the iliac crest, fibula, and scapula; these grafts can be harvested both as vascularized and non-vascularized ones [1, 2, 4]. The possibility of harvesting fibula and scapula was initially ruled out since the process of harvesting these grafts is quite complicated and traumatic. Based on the fact that in our case we needed a relatively small non-vascularized bone graft and considering all the advantages and disadvantages of each method, our priority was given to iliac crest bone graft.
The commonly used sites of iliac crest bone graft harvesting are the anterior and posterior iliac crest. The posterior iliac crest is the source of cancellous and corticocancellous bone, but considering the patient’s incomplete recovered condition, the access to the donor area, and the size of the required bone graft, we gave our priority on the application of the anterior iliac crest. The reported donor-site complications are pain, fracture of the anterior superior iliac spine (ASIS), herniation of abdominal contents, hematoma, injury of the neurovascular bundle, infection, etc. [1, 2]. Due to properly performed intervention and professional postoperative care, we managed to avoid the mentioned complications (Figures 7-9).
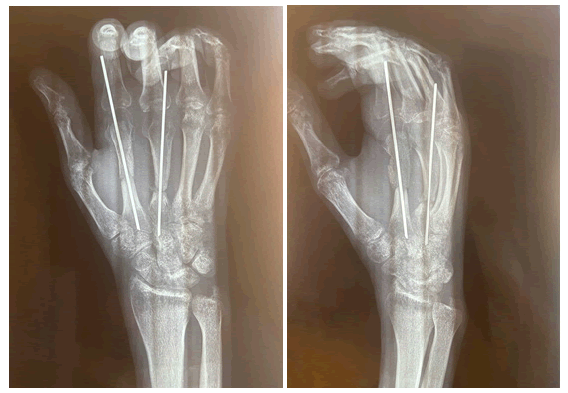
Figure 7:Harvested Anterior Iliac Crest Bone Graft.
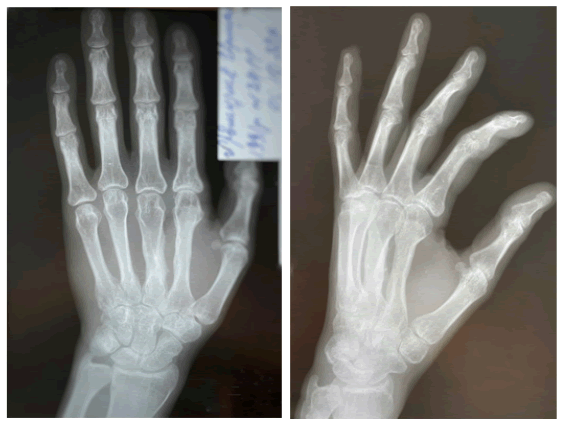
Figure 8: Harvested Anterior Iliac Crest Bone Graft.
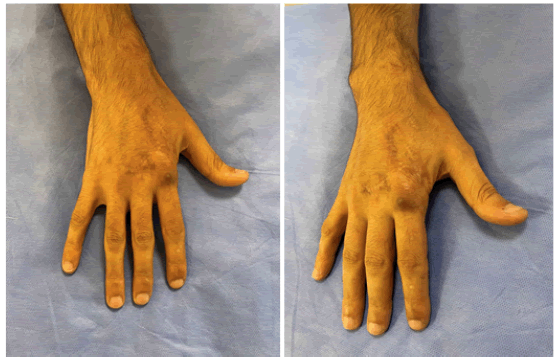
Figure 9:Harvested Anterior Iliac Crest Bone Graft.
Based on the observation data of our clinic from the 27th of September 2020 till the 27th of September 2022, nearly 58,3% (n= 35) of patients with bone defects, had undergone iliac crest bone graft replacement surgery. The presented case shows a remarkable example of the necessity of teamwork, a professional approach, and proper secondary reconstruction. The postoperative radiographs and follow-up demonstrate satisfactory functional and aesthetic results. The last examination was performed on the 28th of November 2022, the patient was able to perform a full range of movements, skin colour was normal, and sensational findings were in the range of normal results. The patient has fully returned to their daily routine and is satisfied with the outcome .
Citation: Sahakyan AB et al, Reconstruction of A Metacarpal Bone After Shrapnel Injury By Using Iliac Crest Bone Graft. Reconstr Surg Anaplastol, 2022, 11(5), 08-10
Received: 18-Oct-2022, Manuscript No. ACR-22-21451; Editor assigned: 25-Oct-2022, Pre QC No. ACR-22-21451 (PQ); Reviewed: 29-Oct-2022, QC No. ACR-22-21451 (Q); Revised: 05-Nov-2022, Manuscript No. ACR-22-21451 (R); Published: 10-Nov-2022, DOI: DOI.10.37532/22.11.5.008-010
Copyright: ©2022 Sahakyan AB, et al., This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.