Review Article - (2023) Volume 12, Issue 2
Ischemic colitis is rarely treated by laparoscopy. The point of this review using of propensity score matched study to compare preoperative with intraoperative character and short-term outcome for severe and urgent cases of ischemic colitis.
Methods techniques: Review survey by retrospective study of 48 patients who undergoing colectomy for urgent ischemic colitis between Mars 2013 and October 2022 (18 by mean of laparoscopy, 30 by means of laparotomy) performed. After examination we compared short term outcomes after using a one to one ratio and nearest neighbor propensity score matching to obtain similar preoperative and intra-operative parameters in each group.
Results: From January 2013 to December 2022, 48 patients went through new colectomy for IC, 18 by means of laparoscopy, 30 through laparotomy. Before penchant score coordinating, genuinely critical higher contrast before affinity score matching among laparoscopy and open strategy in higher APACHE II score (10 versus 7, p<0.001) for the open gathering contrasted with the laparoscopic bunch, separately additionally higher in ASA (ASA 4: 63% vs. 38.8%, p=0.024) likewise. All patients were Favier II or III: There were more patients in the open group who were Favier III (73.3% vs. half, p=0.014) and had all out colonic ischemia (20% vs. 5.5%, p=0.004) (open vs. laparoscopic) There was no measurably massive contrast in CCI (open versus laparoscopic: 1 vs. 2, p=0.772). There was no measurably massive contrast in the extent of patients with entrail condition (open vs. laparoscopic: 43.3% vs. 40%, p=0.656). After penchant score coordinating, the factors were not generally measurably fundamentally divergent in the two (open and laparoscopic) gatherings of 15 patients each.
Ischemic colitis • Laparoscopy • Colectomy • Comorbidity • Anesthesiologists
Ischemic Colitis (IC) characterized by low or lack of blood supply providing and oxygenation to inside circle and ultimately entrail ischemia, the occurrence of IC is extremely serious condition that went from four and half to forty four cases for every hundred south and cases years [1,2].
The seriousness of IC went from gentle answering clinical treatment to cut off need critical hazardous medical procedure that occur as per thickness contribution from superficial mucosal to transmural and full wall thickness affection. With high death rate up to 60% after medical procedure, when transmural or full thickness necrosis happened.
Utilizing of laparoscopy normally elective however as of late, it is utilized for rising transmural necrosis. However, as most patients go through laparotomy in this way, utilizing of laparoscopy is along these lines, uncommon in such circumstances. The point of this study is to demonstrate the benefit of laparoscopy over laparotomy in momentary circumstances.
Patients and methods
From January 2013 to December 2022, all imminent patients treated in Zagagic college careful division went through crisis critical medical procedure for IC after endoscopic biopsy and neurotic assessment. The all character preoperative circumstances, lap. Examination, clinical conditions, intraoperative condition standard attributes and postoperative result information were reflectively recognized and investigated [3]. Signs for the straightforward methodology relying upon the specialist of choice. Patients with just laparotomy or just laparoscopy or begin laparotomy then switched over completely to open laparotomy, the degree of colon resection, anastomosis whenever finished with or without stoma dependent upon the situation, in like manner.
We are grouping level of ischemia as indicated by Favier's level of characterization:
• Degree i (transient and gentle mucosal ischemia).
• Degree ii (mucosal and muscularis ischemia, by and large
thought about reversible.
• Degree iii transmural however (non-reversible transmural
ischemia).
The Charlson Comorbidity File (CCI) and Assessment II (APACHE II) used for computation for every patient. We can perform a medical procedure following 3 days (performed ≥ 3 days) called postponed careful intercession characterized as careful mediation after the underlying side effects. The etiology of IC was individualized as postoperative IC (in no less than 15 days) and between the latter, as occlusive and non-occlusive was. Length of time ventilation and medical clinic term were finished up from the day of crisis until colectomy done for IC. Dead patients were excluded from analysis. If the patients had long clinic stay, the all measurement was recorded at 30 days after the subsequent medical procedure or during the main same clinic stay. Actual complications were reviewed utilizing the Clavien-Dindo score utilized for grouping. Grade III or more prominent is called significant intraabdominal sepsis diagnosed by mechanized tomography (CT) examine. Delayed entrail peristaltic more than seven days characterized (delayed ileus) [4].
Surgical steps or technique of laparoscopic methods for colectomy in patients of ischemic colitis general sedation, lithotomy position, skin shaved by clipper. Umbilical 12 trocar (initial one) presented under vision. Assessment of the all abdominal content, colon assessment and degree of ischemic area. Two trocars on right and two in left of the colon. The colon was analyzed and dissected from horizontal through the white line and afterward division of the impacted region with endo-GIA stapler’s proximal and distal then division of the ischemic part (Figure 1). The mesentery separated by ligasure. The ischemic part removed through umbilical may be finished by essential anastomosis or anticipating stoma by Hartmann's strategy according to the general state of the patients and abdomen washing by worm saline with then let drains (Figure 2).

Figure 1: After colon preparation and analyzation of the colon, the proximal end shows up in the photograph.
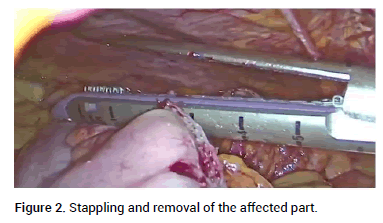
Figure 2: Stappling and removal of the affected part.
We present the information as rate, chi-squared test or Fisher's careful test was utilized for division of information. A propensity score analysis was performed to obtain a one to one match by using the nearest neighbor matching method. The variable from univariate relapse investigation recognized by p values <0.05 that were additionally used to assess the mortality rate [5]. Univariate analysis were included in a wise by good step for multivariate logistic regression analysis to detect the probability of mortality rate for the death rate estimated by ASA, APACHE II score however the degree of gut involved by ischemia estimated by Favier arrangement score. SPSS for Windows (adaptation 25.0; IBM-SPSS Inc., Armonk, N) utilized for all measurable investigations done. For regularly dispersed metric information tried by understudy's t test however none ordinarily date we use Mann-Whitney U test. For the closest neighbor coordinating and balanced match, a penchant score investigation was utilized. The person laparoscopic or open strategy can influence the penchant scores thus; we utilize the different calculated score.
From January 2013 to December 2022, 48 patients went through new colectomy for IC, 18 by means of laparoscopy, 30 through laparotomy. Before penchant score coordinating, genuinely critical higher contrast before affinity score matching among laparoscopy and open strategy in higher APACHE II score (10 vs. 7, p<0.001) for the open gathering contrasted with the laparoscopic bunch, separately additionally higher in ASA (ASA 4: 63% vs. 38.8%, p=0.024) likewise (Table 1). All patients were Favier II or III: There were more patients in the open group who were Favier III (73.3% vs. half, p=0.014) and had all out colonic ischemia (20% vs. 5.5%, p=0.004) (open versus laparoscopic) There was no measurably massive contrast in CCI (open vs. laparoscopic: 1 vs. 2, p=0.772) (Table 2). There was no measurably massive contrast in the extent of patients with entrail condition (open vs. laparoscopic: 43.3% vs. 40%, p=0.656). After propensity score coordinating, the factors were not generally measurably fundamentally different in the two groups (open and laparoscopic) matching of 15 patients each [6].
| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| Open n=30 | Laparoscopy n=18 | P value | Open | Laparoscopy n=15 | P-value | |
| Year of surgery | ||||||
| 2013-2017 | 17 (56.6%) | 7 (48.8%) | 9 (60%) | 6 (40%) | ||
| 2019-2022 | 12 (40%) | 11 (61%) | 6 (40%) | 9 (60%) | ||
| Age | 67 (21-89) | 70 (22-94) | 0.558 | 66 (21-89) | 71 (22-94) | |
| Gender | ||||||
| Male | 11 (36.6%) | (44%) | 0.821 | 8 (53%) | 6 (40%) | 0.789 |
| Female | 18 (61.5%) | 9 (54.8%) | 6 (45%) | 8 (58%) | ||
| BMI (kg/m2) | 24.3 (14.8-38.3) | 22.9 (17.5-30.8) | 0.662 | 24.3 (14.8-30.9) | 22.9 (17.5-30.5) | 0.354 |
| ASA | 0.024 | 0.778 | ||||
| 2 | 4 (1.8%) | 3 (10.2%) | 4 (3.2%) | 1 (6.4%) | ||
| 3 | 9 (29.8%) | 9 (51.2%) | 7 (45.1%) | 6 (48.3%) | ||
| 4 | 19 (63%) | 7 (38.8%) | 8 (53%) | 7 (46.6%) | ||
| 5 | 1 (3.3%) | 0 | 0 | 0 | ||
| CCI | 1 (0-11) | 2 (0-11) | 0.772 | 3(0-10) | 3 (0-11) | 0.208 |
| HTN | 18 (63%) | 10 (61%) | 0.478 | 9 (60%) | 10 (66.6%) | |
| DM | 10 (33.3%) | 7 (38.8%) | 0.935 | 9 (29%) | 11 (35.4%) | |
| CVA | 15 (26.3%) | 7 (17.9%) | 0.338 | 1 (6.6%) | 1 (7%) | |
| CAD | 2 (7%) | 3 (16.6%) | 0.187 | 1 (7%)%) | 3 (0.2%) | |
| Malignancy | 10 (36.5%) | 7 (38.8%) | 0.872 | 7 (46.6%) | 11 (25.4% | |
| APACHE II | 10 (3-23) | 7 (3-23) | <0.001 | 7 (3-12) | 7 (3-23) | 0.522 |
| Surgical delay (= 3 days) | 18 (60%) | 8 (44%) | 0.121 | 1 (66.6%) | 8 (50.3%) | 0.123 |
| Etiology of ICU postoperative IC | 11 (36.6%) | 7(38.8%) | 0.872 | 4 (26.6%) | 6 (40%) | 0.421 |
| Vascular surgery | 7 (23%) | 2 (11%) | 3 (20%) | 2 (13%) | ||
| Other surgery | 8 (14.0%) | 11 (28.2%) | 4 (12.9%) | 8 (25.8%) | ||
| Others etiology | 18 (63.%) | 11 (61.1%) | 11 (73%) | 9 (60%) | ||
| Occlusive | 8 (26.0%) | 5 (27.7%) | 4 (270%) | 4 (27%) | ||
| Nonocclusive | 8 (26.6.0%) | 6 (33.3%) | 6 (40%) | 5 (33.3%) | ||
| Note: BMI: Body Mass Index; ASA: American Society of Anesthesiologists; CCI: Charlson Comorbidity Index; HTN: Hypertension; DM: Diabetes Mellitus; CKD: Chronic Kidney Disease; CAD: Coronary Artery Disease; CVA: Cerebrovascular Accident; and APACHE: Acute Physiology and Chronic Health Evaluation. From: Laparoscopic versus open emergent colectomy for ischemic colitis: a propensity score-matched comparison |
||||||
Table 1. Patient characteristics.
| Unmatched | Matched | |||||
|---|---|---|---|---|---|---|
| Open | Laparoscopy | P value | Open | Laparoscopy | P value | |
| Favier’s classification | 0.014 | 0.6 | ||||
| 1 | 0 | 0 | 0 | 0 | ||
| 2 | 7 (23.3%) | 9 (50%) | 5 (33.3%) | 6 (40%) | ||
| 3 | 22 (73.3%) | 9 (50%) | 10 (66.6%) | 9 (60%) | ||
| Perforation | 13 (43.3%) | 8 (44.0%) | 0.656 | 6 (40%) | 5 (33%) | 0.43 |
| Ischemia site | 0.004 | 0.175 | ||||
| Segmental | 8 (26.6%) | 10 (55%) | 7 (46%) | 8 (53%) | ||
| Right colon | 7 (23%) | 1 (5.5%) | 3 (20%) | 1 (6.6%) | ||
| Left colon | 9 (30%) | 7 (38.8%) | 4 (27.0%) | 5 (33.3%) | ||
| Total | 6 (20%) | 1 (5.5%) | 0 | 1 (6.6%) | ||
| Small bowel ischemia | 5 (16.3%) | 4 (22%) | 0.512 | 4 (26.6%) | 0.497 | |
| Surgical procedure | 0.014 | 0.25 | ||||
| Hartmann | 26 (90%) | 14 (77.7%) | 13 (86.60%) | 12 (80%) | ||
| Anastomosis with stoma | 1 (1.8%) | 0 | 1 (3.2%) | 0 | ||
| Double barrel stoma | 2 (6.06%) | 5 (27.7%) | 1 (7%) | 3 (20%) | ||
| Blood loss (cc) | 100 (30-3500) | 50 (30-1600) | 0.326 | 50 (30-1699) | 0.469 | |
| Conversion | 7 (23.3%) | - | 3 (21%) | |||
| Operation time (min) | 200 (120-360) | 180 (120-600) | 0.66 | 180 (120-360) | 180 (120-420) | |
| Laparoscopic vs. open emergent colectomy for ischemic colitis: A propensity score-matched comparison | ||||||
Table 2. Perioperative details. Laparoscopic versus open emergent colectomy for ischemic colitis: A propensity score matched comparison.
Data are summarized in Table 3. Before propensity score coordinating, patients with higher extent of intra-abdominal septic collection (47% vs. 16%, p=0.003), likewise complication identified more in patients in the open group (half vs. 22.2.0%, p=0.004), higher mortality (49.1% vs. 20.5%, p=0.004), and longer hospitalization (32 days vs.19 days, p=0.001). After propensity score matching, patients undergoing open (vs. laparoscopy) had longer ventilator support (20 days vs. 0 days, p<0.001), more significant complication 77% vs. 44%, p=0.001), patients required longer ventilator support (14 days vs. 3 days, p=0.039), likewise going through open (vs. laparoscopy) had more complication (half vs. 22%, p=0.030) and outstanding, there was a pattern toward less intra-abdominal sepsis (38.7% vs. 19.4%, p=0.093) and more limited emergency clinic stay (32 days vs. 20 days, p=0.061). In any case, there was not measurably tendency to fewer abdominal sepsis (66% vs. 47.5%, p=0.200) or mortality (40% vs. 26.6%, p=0.277) [7].
| Matched | Unmatched | |||||
|---|---|---|---|---|---|---|
| Open | laparoscopy | P value | Open | laparoscopy | P value | |
| Surgical site complication | 15 (50%) | 4 (22.20%) | 0.004 | 7 (46.5%) | 3 (20%) | 0.03 |
| Prolonged ileus (%) | 11 (36.6%) | 4 (22.2%) | 0.087 | 5 (33.4%) | 4 (27.0%) | 0.587 |
| Intra-abdominal abscess | 14 (47%) | 3 (16.6%) | 0.003 | 6 (40%) | 3 (20%) | 0.093 |
| CVA | 2 (6.6%) | 1 (5.7%) | 0.851 | 1 (6.6%) | 1 (6.6%) | 0.1 |
| Heart | 7 (23.3%) | 2 (11.3%) | 0.114 | 2 (13%) | 1 (8.6%) | 0.688 |
| Kidney | 9 (3%) | 2 (11%) | 0.023 | 2 (13%) | 1 (6.6%) | 0.39 |
| Ventilator support | 0 (0-118) | 0 (0-40) | <0.001 | 14 (0-118) | 3 (0-40) | 0.039 |
| Reoperation | 7 (23.7%) | 8 (22%) | 0.643 | 2 (13.9%) | 3 (2%) | 0.74 |
| Ischemia | 2 (6.60%) | 1 (6.7%) | 1 (3.2%) | 2 (13.3%) | ||
| Bowel perforation | 2 (6%) | 1 (5.5%) | 1 (3.2%) | 1 (3.2%) | ||
| Bleeding | 1 (1.8%) | 1 (2.6%) | 0 | 1 (3.2%) | ||
| PAD | 4 (13%) | 1 (2.6%) | 0.091 | 2 (13%) | 0 | 0.039 |
| Major complications | 23 (77%) | 8 (44%) | 0.001 | 10 (66.5%) | 15 (47%) | 0.2 |
| Mortality | 15 (50%) | 4 (22%) | 0.004 | 6 (40%) | 4 (26.6%) | 0.277 |
| Hospital stay (days) | 32 (4-139) | 19 (11-75) | 0.001 | 32 (19-139) | 20 (11-75) | 0.061 |
| Note: CVA: Cerebrovascular Accident; PAD: Percutaneous Abscess Drainage | ||||||
Table 3. Postoperative outcome.
In univariate examination Favier's scoring (p=0.017), and trans parietal colonic ischemia (p=0.004) were measurably critical related with mortality. Additionally in univariate examination, ASA class (p=0.005), CCI (p=0.009), APACHE II score (p<0.001), laparoscopy approach (p=0.006), aorta related a medical procedure (p=0.017), after multivariate examination, CCI (p=0.024), APACHE II score (p=0.001), Favier's grouping (p=0.023) were free indicators of mortality (Table 4) [8].
| Univariable | Multivariable | |
|---|---|---|
| Age | ||
| Years of operation | 2019-2022 0.90 (0.39-2.04, p=0.792) | |
| BMI | 1.02 (0.99-1.04, p=0.344) | |
| Gender | 1.04 (0.95-1.17, p=0.305) | |
| Male | ||
| Female | 0.59 (0.26-1.40, p=0.237) | |
| ASA | ||
| 2,3 | ||
| 4,5 | 3.7 (1.48-9.11, p=0.005) | 0.21 (0.31-1.17, p=0.074) |
| APACHEII | 1.39 (1.17-1.43, p<0.001) | 1.35 (1.10-1.41, p=0.001) |
| Surgical delay | 1.30 (0.61-3.22, p=0.429) | |
| Laparoscopy | 0.28 (0.11-0.68, p=0.006) | 0.59 (0.16-2.33, p=0.466) |
| Aorta related surgery | 4.56 (1.32-16.52, p=0.017) | 2.07 (0.40-10.72, p=0.383) |
| Etiology of ICU | ||
| Postoperative ICU | ||
| Other etiology | ||
| Faviers classification | 76 (0.32-1.76, p=0.51) | |
| 2 | ||
| 3 | 7.5 (1.32-16.52, p=0.017) | 9.01 (1.35-60.37, p=0.023) |
| Total ischaemia | 7.21 (1.86-28.79, p=0.004) | 3.86 (0.55-27.80, p=0.174) |
| Conversion | 0.80 (0,19-3.50, p=0.786) | |
| Note: BMI: Body Mass Index; ASA: American Society of Anesthesiologists; and APACHE: Acute Physiology and Chronic Health Evaluation. | ||
Table 4. Predictive factors for mortality in patients with ischemic colitis.
We make correlation of rising laparoscopic versus open colonic resection of instances of urgent ischemic colitis by the propensity score matching that identify the span of ventilation support and careful site of sepsis that were measurably fundamentally diminished after the laparoscopic approach [9]. We found in clinic stay, unsignificant, or mortality had no measurably huge distinction. After multivariate examination, APACHE II score (OR=1.25, p=0.001), CCI (OR=1.29, p=0.024), and Favier's arrangement score (OR=9.02, p=0.023) that remained measurably huge indicators information of mortality.
Estimating the “causal” factor on results of randomized clinical cases management. That acknowledged as the highest quality level system, as no time for diagnosis. Likewise IC is uncommon cases for time of randomization; hence. The advantage of propensity score matching correlation between treated that noticed lower [10,11].
The perioperative mortality might ultimately depend on 60% after medical procedure that are a result of many elements that related with age, generate status, partner comorbid infection (heart, lung and diabetes) or the level of ischemia itself and contribution of encompassing affected site of tissues. In our concentrate no measurably huge difference after propensity score coordinating, in Favier's order, area of ischemia by involved in propensity score. In any case, in 2013, Reissfelder, et al. introduced many score factors as renal warmth, non-occlusive IC, degree of inside ischemia, serum lactate and span of catecholamine level.
We don't utilize these variables that excluded from our coordinating; the laparoscopy is generally utilized in elective colon medical procedure however not in that frame of mind as smooth postoperative, less timing and using additional endoscopy that was dangerous yet endoscopy benefit of good representation of all colon and benefit of biopsy. As indicated by hole by laparoscopy, the ACS-NSQIP information base review, just 125 of 4548 (4.3%), after IC colectomy had whole and fecal fistula. Most distributed examinations on in patients after the laparoscopic approach is good diagnosis. Furthermore, decline the careful site complication rate. In the developing setting by these examinations after laparoscopic approach however decrease ventilation Tolmie, sepsis, or medical clinic stay.
Side effects of IC are many times vague clinically particularly beginning phase as peritonitis shows up just in little quantities of patients additionally not present in lethargic or severe pain. Patients in ICU, must be suspected in patient not response to treatment likewise laparoscopy can see regularly from patients deny diet as transmural ischemia can exist. Without clinical signs, laparoscopic assessment could be an early symptomatic apparatus. When we compared the surgical time operation between the laparoscopic and open groups, we found that the delaying and longer in the open group than in the laparoscopic group 44% vs. 60%, p=0.121; after inclination, (50.3%, vs. 66.6% p=0.123). However, this finding had no significant differences but the job of laparoscopy as an early demonstrative of the intense using further (EAES conference) [12].
In our review we were done the all our length of operation (in open technique: 200 min, versus in laparoscopy strategy: 180 min, with (p-value=0.693). But it is opposed to cases on managing diverticulitis the time among open and laparoscopy was not huge, One explanation may be that medical procedure for IC could have been more complicated as certain specialists get some margin to close a laparotomy contrasted with more experience laparoscopic surgeon careful make destinations.
Had huge signs, Maggiore and pains concluded same result in progress in open and laparoscopic medical procedure for serious intense colitis in the event that was related with a comparable condition. Sampietro, et al. covered 145 patients oversaw by early laparoscopy for subtotal colectomy for ulcerative colitis or Crohn's illness they found it was protected and practical for intense cases. After a laparoscopic or laparotomy we like to make second look by laparoscopy after 24 h-72 h. We suspect vascular abnormalities that Found the beginning as the association between the center colic and left colic supply routes might be variable (Griffith's point) in up to 48% of patients between distal sigmoid and superior rectal arteries course. Additionally past colectomy or aortic medical procedure can change the vascular life structures of the colon and segmental life structures [13-17].
Past investigations have viewed different research facility boundaries as related with mortality, like LDH>500 U/l, Blood Urea Nitrogen (BUN) (>30 mg/dl), Hb<11 g/dl, and hyponatremia (Na<138 mEq/l). In our review the overall actual status of the, were set by APACHE II score, that (OR: 1.25, 95% CI 1.10-1.41, p=0.001) as percent variable for mortality. With an AUC of 0.86 (77.9-94.1, p<0.001), the APACHE II was high prescient worth. Whenever contrasted and Peixoto, et al. that found AUC was 0.89. Degree with colectomy, lactate level and kidney function that can happened if the condition last >12 h. On the other hand, a few creators found the reason for IC didn't to elements of postoperative mortality.
After propensity score coordinating, numerous change done as a result of peritonitis, serious complication ,and diffuse adhesion and fecal fistula and peritonitis was 7/18=23.3%. [18,19].
Our review has a few restrictions:
• Due to the review plan not precise 100 percent as,
different variables might have influenced the postoperative
results, including entrail distension. General circumstances,
crippling elements, or intraoperative waste spillage.
• The example size of patients was little (pre affinity, n=48;
post inclination, n=30).
• The choice to play out the laparoscopic activity need
specialist encounters subordinate.
• Besides, specialist choice for level of resection is selfexperience
choice may be varied from specialist to other
for essential anastomosis.
Last, just realized many factors not estimated in these review. Randomized study would be hard to perform. At last, the time span of this study was long, had many advances in careful procedures and technique, for example, working time, intensive care which might have affected the careful results (postoperative clinic stay and complication rate) [20].
Laparoscopic should be prepared in rising condition, for example, urgent colectomy after early symptoms IC as it is attainable and protected, less postoperative careful site complication and less medical clinic stay and ventilation support time whenever contrasted with open laparotomy. The significant complication that leads to death rates in view of the seriousness of illness and patient status, however the benefits of laparoscopic colectomy is decrease of for patients mobility and mortality but yet need additionally considered and more randomized cases for studies.
None to declare.
HA: Conceptualization, formal analysis, investigation, methodology, software, validation, writing original.
HS: Draft, editing, supervision: formal analysis, SN investigation, methodology, validation, editing.
MA: Formal analysis, investigation.
AY: Methodology, validation, editing.
IB: Conceptualization.
ME: Formal analysis, investigation, methodology, software, validation.
HA: writing original draft, editing, supervision. All authors read and approved conception the final manuscript.
• Ethical approval from our university by NO.
• Approval consent to participate and consent for publication
• All the authors interested and approved the present manuscript.
• No Competing interests
• Available data and materials included in the article that available
and under requesting.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Eraki ME, et al."Open Versus Laparoscopy in Management of Urgent Colectomy for Severe Ischemic Colitis Using a Propensity Score Matched in Comparison ". Reconstr Surg Anaplastol, 2023, 12(1), 1-7.
Received: 26-Dec-2022, Manuscript No. ACR-22-21165 ; Editor assigned: 29-Dec-2022, Pre QC No. ACR-22-21165 (PQ); Reviewed: 12-Jan-2023, QC No. ACR-22-21165 ; Revised: 31-Mar-2023, Manuscript No. ACR-22-21165 (R); Published: 07-Apr-2023, DOI: 10.37532/ acr.23.12.1.001-007
Copyright: © 2023 Eraki ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.