Case Report - (2024) Volume 15, Issue 3
Chronic limbic encephalitis can be a major source of morbidity in patients with T1DM. The aim of the case report is to highlight the significance of early identification of signs of memory impairment in patients with T1DM, screening for GAD65 antibodies in the CSF and to be aware of the possible association between limbic encephalitis, GAD65 antibodies and type 1 DM. Limbic Encephalitis (LE) is an inflammatory condition affecting the brain's limbic system, which includes regions critical for memory and emotion.
Diabetes • Limbic encephalitis • Antibodies • Medicine
The disorder is often linked to autoimmunity, where the immune system mistakenly targets brain cells, leading to symptoms like seizures, memory loss, and psychiatric disturbances. Among the autoimmune markers, Glutamic Acid Decarboxylase 65 (GAD65) antibodies are significant. These antibodies target the GAD65 enzyme, crucial in producing Gamma-Aminobutyric Acid (GABA), an essential neurotransmitter [1]. The presence of GAD65 antibodies has been observed in several autoimmune conditions, including Type 1 Diabetes Mellitus (T1DM).
Type 1 diabetes mellitus is characterized by the immune system's attack on insulin-producing beta cells in the pancreas, leading to chronic high blood sugar levels. The association between T1DM and GAD65 antibodies is well-documented, indicating a common autoimmune pathway. Recent studies suggest a potential overlap between LE and T1DM through these shared antibodies, indicating a more systemic autoimmune dysregulation.
Connecting these dots, researchers hypothesize that the presence of GAD65 antibodies in both conditions suggests a broader spectrum of autoimmune responses. Understanding this relationship could pave the way for better diagnostic markers and therapeutic strategies, offering hope for more comprehensive management of patients suffering from these debilitating autoimmune disorders [2].
Limbic encephalitis involves inflammation involving the structures of the limbic system (e.g. limbic cortex, amygdala, hypothalamus, hippocampus, cingulate gyrus,). It may be a paraneoplastic phenomenon or a sequel of autoimmune encephalitis. The possible association of GAD65 related limbic encephalitis and type 1 DM remains an under reviewed subject. The purpose of this case report and subsequent literature review, is to highlight the possible association of limbic encephalitis and type 1DM, and the need for early identification and treatment of patients presenting with anterograde amnesia or seizures in the setting of limbic encephalitis [3].
Here, we present a case of a 21 year old indigenous girl, who was first brought to the hospital at the age of 15 years, with the complaint of anterograde amnesia for three to six months. This is on a background of T1DM and hypothyroidism, diagnosed at the age of two. Patient had poor glycaemic control on a background of erratic social life. Patient also reported visual hallucinations at one point [4]. Nil behaviour and mood disturbances were documented at the time (Figure 1).
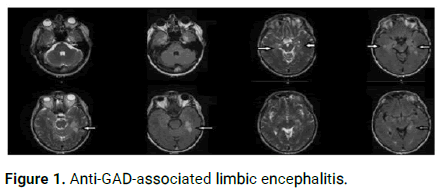
Figure 1: Anti-GAD-associated limbic encephalitis.
Anterograde amnesia was thoroughly investigated. MRI showed marked atrophy involving both hippocampi and temporal lobes; nil changes with contrast were seen. EEG was unremarkable. Lumber puncture was positive for oligoclonal bands. GAD65 antibodies were not tested in the CSF. Anti-Hu, Anti yo, anti Ri antibodies were negative. Nil evidence of malignancy could be found and a diagnosis of chronic limbic encephalitis likely secondary to autoimmune process was made. She was treated with 3 days of IV immunoglobulin and methylprednisolone with nil significant improvement. She was discharged with follow-up in memory clinic and establishing several supports in place. Patient had a second hospital admission for anterograde amnesia, 5 months after the first admission [5]. Nil new findings were identified. It was advised that the disease was likely a pervasive and nonremitting process and nil long term improvement was expected. The 2nd Lumber puncture had GAD65 antibodies reported.
Since then the patient has had several admissions for DKA in the setting of poor compliance with insulin. Anterograde amnesia continues to be an issue. Moreover, labile mood with emotional outburst is now a very prominent part of the presentation.
The presentation of patients with limbic encephalitis can range from amnesia, cognitive impairment, seizures, and agitation to mood and behavior changes. Gagnon and Savrd, with a review of 58 cases of limbic encephalitis, demonstrated that the most common presentation in patients with LE was seizures, followed by anterograde amnesia [6].
Association of GAD65 antibodies to limbic encephalitis has been reported in several case reports. Although the pathophysiology of GAD65 autoimmune encephalitis has been under debate, the most commonly accepted mechanism remains the inhibition of enzyme GAD65 in the CNS by the autoantibodies, resulting in reduced conversion of glutamate into GABA. GABA is widely used in the central nervous system as an inhibitory neurotransmitter [7]. This reduction in the synthesis of GABA, with or without reduction in the release of GABA ergic presynaptic vesicles, tips the balance, augmenting the dominance of excitatory neurotransmitters precipitating epileptogenic activity.
Malter, et al. reviewed 138 cases of limbic encephalitis with positive GAD65 antibodies and concluded that markedly elevated GAD65 antibodies define a form of non paraneoplastic LE. Akin, et al. reported a case of a 16 year old boy who was diagnosed with T1DM, six months after being admitted for an episode of limbic encephalitis with positive GAD65 antibodies in the CSF. Elevated antibody titres of GAD65 antibodies in the CSF are also associated with other neurological presentations including epilepsy, cerebellar ataxia and stiff-personsyndrome. Low titres of serum GAD antibodies may be seen in healthy individuals and account for up to 80% of patients with type 1 diabetes mellitus. Interestingly, T1DM increases the risk of Epilepsy by 4%-6% compared to the general population, and patients with epilepsy have a four times increased prevalence of T1D than the general population.
T2/Fluid-Attenuated Inversion Recovery (FLAIR) hyperintensity in the medial temporal lobes on MRI may be seen in 80% of patients with Limbic encephalitis. Contrast enhancement in these regions is very rare [8]. PET scan demonstrates hypermetabolism in the medial temporal lobes, hypometabolism may be seen later in the course of the disease CSF findings include pleocytosis, elevated protein and abnormal oligoclonal bands. High titre of GAD65 may also be found in the CSF. EEG may show generalized or focal slowing with or without epileptiform activity, most dominantly in the temporal regions.
Different management approaches have been used widely for the treatment of GAD65 positive limbic encephalitis [9]. A review of 58 cases of limbic encephalitis with GAD65 antibodies by Gagnon and Savrd showed that most patients do not see a complete resolution of symptoms. This was also seen in our patient as 10 years after her first admission with limbic encephalitis, she was still suffering from short term memory impairment, cognitive impairment and mood disturbances.
Several different treatment modalities with varying treatment duration and follow up ranging from 0-96 months have been used. Commonly used treatments included steroids, immunoglobulin, plasma exchange, rituximab, cyclophosphamide, steroid sparing agents including azathioprine and Mycophenolate Mofetil [10]. No studies re currently available to ascertain the superiority of one treatment over another.
GAD65 associated limbic encephalitis in patients with type 1 DM remains an understudied subject. Patients presenting with limbic encephalitis with GAD65 antibodies may need monitoring for possible development of type 1 diabetes mellitus and vice versa. Further trials would be beneficial in identifying a diagnostic approach and best treatment guidelines for early detection and management of patients with GAD65 associated limbic encephalitis.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Fishan N. "Limbic Encephalitis, Type 1 Diabetes Mellitus and Gad65 Antibodies, Have We Connected the Dots?". J Diabetes Metab, 2024, 15(3), 1-2.
Received: 21-May-2020, Manuscript No. JDM-24-4329; Editor assigned: 26-May-2020, Pre QC No. JDM-24-4329 (PQ); Reviewed: 09-Jun-2020, QC No. JDM-24-4329; Revised: 15-May-2024, Manuscript No. JDM-24-4329 (R); Published: 12-Jun-2024, DOI: 10.35248/2155-6156.10001099
Copyright: ©2024 Fishan N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.