Review Article - (2023) Volume 9, Issue 2
In patients with end-stage kidney disease, renal transplantation has been found to significantly improve reproduction in women of childbearing age (18-49 years). However, despite the significant improvements in renal transplants and obstetric care, renal transplant recipients are drastically more susceptible to adverse maternal, fetal and allograft function outcomes in comparison to their non-transplant counterparts.
Preeclampsia is a hypertensive, multi-system complication that occurs in 2%-8% of all pregnancies and is a major cause of both maternal and fetal morbidity and mortality worldwide. The diagnosis of preeclampsia is defined by the new onset hypertension after 20 weeks of gestation in a previously normotensive pregnant woman with one of the following new onset proteinuria, other evidence of maternal organ dysfunction, including renal insufficiency, liver dysfunction, pulmonary edema, cerebral abnormalities and thrombocytopenia. Preeclampsia has an increased prevalence in renal transplant recipients, with a reported incidence that is 5%-6% higher in post-transplant pregnancy when compared to non-transplanted pregnancy. An estimated 52%-69% of renal transplant recipients have pre-existing hypertension prior to pregnancy, increasing their risk of superimposed preeclampsia developed. Preeclampsia predisposes the mother and child to future complications such as diabetes, hyperlipidaemia, cardiovascular disease, graft failure and end-stage renal disease.
Bacillary angiomatosis • Bartonella • Human immunodeficiency virus • Infection • Dermatopathology
The current literature regarding preeclampsia development in renal transplant recipients remains scarce, with the underlying pathophysiology being poorly understood. Similar gaps in the literature are apparent for numerous adverse maternal outcomes. A few studies have thoroughly evaluated renal transplantation as a risk factor for not only preeclampsia development but for other adverse pregnancy complications. The current studies available that discuss pregnancy outcomes in post renal transplant patients are solely limited to observational studies, case reports and voluntary registries.
This identifies a large gap of knowledge as the evidence from these type of publication is weak. In this review article we will try to extract strong evidence from the literature to discuss risk factors for developing preeclampsia in transplant recipients.
Aim
The primary aim of this literature review is to identify the factors that may increase the incidence of preeclampsia in renal transplant recipients and present as potential predictive markers.
Objectives
This review will discuss several potential risk factors for preeclampsia development post renal transplant, with the following being the primary focus of the data extraction.
Risk factors related to underlying maternal factors:
• Maternal age
• Pre-pregnancy renal function
• Pre-pregnancy hypertension
• Pre-pregnancy diabetes mellitus
• Pre-pregnancy proteinuria
• Risk factors related underlying renal
transplantation:
• Transplant to pregnancy interval
• Type of donor
• Reason for transplantation
• Use of immunosuppression medications
Study design
The clinical question was constructed around the aims of the study, allowing for the identification of specific key words to be implemented in the search strategy. A thorough literature search was done using these relevant key terms and reputable literature databases [1]. The list of relevant literature that met the inclusion criteria and was reviewed for the predictive risk factors, including maternal and transplantation, in the development of preeclampsia. Any reported similarities and differences between studies were noted, with these being further analysed to conclude their level of evidence.
A thorough systematic literature search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for both systematic reviews and meta-analyses (Figure 1).
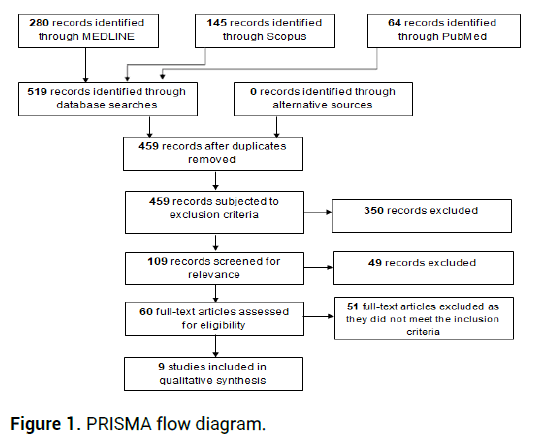
Figure 1: PRISMA flow diagram.
Search strategy
The PICO framework was used to form the research question as to the focus of this literature review and assist in identifying the key terms to be used in the literature search. The PICO framework enabled the following appropriate terms to be distinguished.
• Population: Pregnant women
• Intervention: Post renal transplant
• Comparison: Preeclampsia
• Outcome: Risk factors post renal transplant
Using the following keywords pregnancy, post renal transplant, risk factors and preeclampsia, the literature databases MEDLINE, including CINAHL Complete, MEDLINE Complete and Open Dissertations and MEDLINE, Scopus and PubMed, were searched to derive a list of relevant literature. Boolean logic was also applied to combine search terms and refine the output of the literature generated. Once duplicates were removed, the titles and abstracts of the remaining records were screened to ensure relevance according to the inclusion and exclusion criteria. This reaped an exclusive list of studies that could be evaluated for data extraction and analysis. The literature search was conducted and the records acquired on the 1st of March 2021, with the bibliographies of these references being screened on the 2nd of March 2021. Articles were then critically appraised using CASP tool and levels of evidence.
Inclusion and exclusion criteria
The list of records collected was screened for eligibility and relevance according to the inclusion and exclusion criteria, which are as the following:
Inclusion criteria:
• Renal transplant
• Presence of preeclempsia during pregnancy
• Risk factors for preeclempsia discussed
• Literature published after 2000
• Published in English language
• Peer-reviewed literature
Exclusion criteria
• Non pregnant women
• CKD other than renal transplant
• Multiorgan transplants
• Literature published prior to 2000
• Published in any non English language
• Case studies
The scope of publication was narrowed down to the past 20 years to eliminate inaccurate data due to recent advances in the understanding of the pathophysiology of preeclampsia and hence the diagnosis and management. The focus of this literature review will solely be on studies that evaluated renal transplants in pregnant women, with the presence of preeclampsia during pregnancy being identified and the specific risk factors being discussed. Presence of CKD other than renal transplant and multiple organ transplants will be excluded to avoid data unrelated to the primary research question [2]. Furthermore, only papers published in the English language were included in this review to reduce any inaccuracies that may potentially arise as a result of misinterpretation through translation. Case studies were excluded due to their lack of ability to generalize and risk of over-interpretation.
Data extraction and analysis
For each study included in this review, the maternal factors and renal transplantation associated risk factors were identified and analysed [3]. The following set of questions were employed to thoroughly evaluate the data provided in each study identified following the search strategy in this review.
Questions
• What are the predictors that may increase preeclampsia in
pregnant renal transplant recipients?
• What are the most common risk factors for preeclampsia post
renal transplant?
• Are there additional risk factors for preeclampsia post renal
transplant compared to those found in nonrenal transplant
pregnancies?
• Will the presence of these predictors prior to transplant
increases the risk of developing preeclampsia compared to
having these predictors occur post renal transplant?
• Can we rely on these predictors for the prevention of
preeclampsia?
Overall findings of the reviewed articles
Majak, et al., conducted a retrospective cohort study to identify the clinical characteristics predictive of preeclampsia in 175 pregnancies, with a preeclampsia diagnosis being established in 65 of these cases. Three predictive factors were identified in this study: Chronic hypertension, previous preeclampsia and elevated serum creatinine, all presenting at the start of the patient’s pregnancy [4]. The risk of preeclampsia development was also presented, with the results suggesting a risk of 19% if none of the above factors were present, 45%-59% if one was present, 80%-87% if two were present and 96% if all three were present. Inclusively, these findings provide evidence that the risk of preeclampsia development in pregnant women who have previously received a renal transplant can be predicted with the discussed prognostic factors, which are easily identifiable at the start of the pregnancy [5].
Vannevel, et al., reported whether preeclampsia is associated with kidney function decline either during the pregnancy or in the long term. The pregnancy outcomes and longterm renal outcomes were evaluated in 52 women, including short and long-term graft outcomes and renal function at conception. The data revealed that chronic hypertension was present in 27% of participants at baseline. The mean estimated glomerular filtration rate was 52.4 mL/min/1.73 m2 at the start of pregnancy, a significantly different value to that at the time of delivery, 47.6 mL/min/ 1.73 m2. Twenty women presented with preeclampsia, with the decrease in glomerular filtration rate being significantly greater between conception and delivery, when compared to the 62% of women who did not develop preeclampsia [6]. The follow-up period of glomerular filtration rate was noted at a median value of 5.8 years, with the mean estimated rate being 38 mL/min/1.73 m2 at the final follow-up. Overall, this retrospective cohort study provides evidence that preeclampsia is prevalently associated with pregnancy complications after renal transplantation; however, it is not associated with any long-term renal dysfunction.
Tebet, et al., assessed the laboratory markers and renal function in pregnant women post-renal transplantation. In addition to an evaluation of maternal and fetal data, in 43 women. The findings of this cross-sectional prospective study demonstrated a gradual increase in serum creatinine levels, proteinuria, urinary protein/creatinine ratio and albumin/ creatinine ratio during pregnancy. Moreover, these results revealed that the sensitivity and specificity of protein/creatinine in predicting the occurrence of preeclampsia was significantly high at 96% and 94%, respectively. The remaining renal factors: Elevated serum creatinine levels, urinary albumin/creatinine ration and retinol-binding protein levels, were associated with prematurity in the third trimester [7]. This study also reported that preeclampsia was the primary cause of renal function decline, in 65% of cases, at the end of the patient’s pregnancy. Although not providing any conclusive findings, this study provides evidence for the use of proteinuria, urinary protein/creatinine ratio and retinol-binding protein levels as preeclampsia prognostic markers in pregnant women post-renal transplantation.
An additional study by Majak, et al., assessed obstetrical and neonatal outcomes in 119 women in their first pregnancy who had previously received a kidney transplant. These data were then compared to 238 first deliveries in non-transplanted women. The findings revealed a significant increase in the risk of preeclampsia in the kidney transplant group when compared to the non-transplant women. Moreover, the development of preeclampsia in the women who had received a kidney transplant was early onset, being diagnosed at less than 34 gestational weeks, in 50% of cases. The risk of caesarean delivery, preterm delivery, and birthweight below the 10th centile was largely increased in the kidney-transplanted women. Of the women in the kidney-transplanted group who presented with chronic hypertension at the beginning of their pregnancy, 63% of these developed preeclampsia, indicative of chronic hypertension being a pertinent risk factor [8]. These findings provide evidence and concurs the current literature that the incidence of preeclampsia is significantly increased during pregnancy in women who have previously received a kidney transplantation. Furthermore, this study suggests that chronic hypertension is a predictive risk factor for the development of preeclampsia in these women.
You, et al., retrospective cohort study aim was to determine the most crucial factor for the prediction of these adverse pregnancy outcomes in renal recipients. In this study, a vast number of outcomes were reviewed, including pregnancy outcomes, possible predictive factors, including pre-pregnancy serum creating, prepregnancy proteinuria, transplantation-pregnancy interval and type of immunosuppressants. Adverse pregnancy-related outcomes were defined as conditions including preeclampsia, fetal growth restriction, prematurity before 34 weeks of gestation, fetal loss and graft dysfunction during pregnancy or within three months from delivery. The findings of this study suggest that pre-pregnancy serum creatinine is the sole factor associated with adverse pregnancy outcomes, with 1 mg/dL being determined as the cutoff for the prediction of these adverse outcomes. The evidence provided to support this was the 7.7 times increased risk of preeclampsia in participants with a pre-pregnancy serum creatinine of greater than 1 mg/dL. The conclusion was that pregnancy serum creatinine is the most prominent predictive factor for adverse pregnancy outcomes.
Hassan, et al., compared the outcome of pregnancy in patients who had previously undergone a renal transplantation within 24 months prior to becoming pregnant and those who became pregnant over 24 months after renal transplantation. The study population included 44 patients, 24 in the over 24 months group (A) and 20 in within 24 months group (B). The primary outcomes measured were serum creatinine and the 24-hour urinary protein concentration, with these data points being measured at each trimester. Additionally, the incidences of both preeclampsia and gestational diabetes were recorded in each patient throughout their pregnancy. An increase in the incidence of preeclampsia was also seen between the two groups, 25% in group A and 30% in group B; however, the difference was not statistically significant. In conclusion the findings of this study support the hypothesis that a longer interval between renal transplantation and pregnancy is correlated with a better pregnancy outcome.
Kovac, et al., analysed pregnancy and kidney function in 18 women with transplanted kidneys, with the primary outcome measures being serum creatinine before and after pregnancy, the median duration of pregnancies, the incidence of preeclampsia and other pregnancy factors, including delivery by caesarean. The findings revealed reduced serum creatinine levels prior to conception when compared to three-year post-delivery. Delivery by caesarean was conducted in 86% of cases. The incidence of organ rejection was also discussed, with no rejections occurring during the pregnancy itself; however, three rejections were reported within the first nine months post-delivery. These findings suggest that renal function and proteinuria does not deteriorate in pregnant women after kidney transplantation in the three-year period assessed post-pregnancy; however, rejections in the early post-pregnancy period were prevalent (13.6%). Moreover, the incidence of preeclampsia was significantly greater than the expected frequency in the average population, providing evidence that renal transplantations increase the likelihood of preeclampsia in pregnant women. The final two studies included in this review followed a systematic review and meta-analysis study design.
Shah, et al., conducted a thorough literature search to estimate the pooled incidence of pregnancy outcomes, maternal complications and fetal complications in kidney transplant recipient pregnancies across the globe. A total of 87 full-text articles were evaluated, representing 6712 pregnancies in 4174 kidney transplant recipients. The incidence of pregnancy outcomes and complications are as follows: Induced abortions (12.4%), miscarriages (15.4%), stillbirths (5.1%), ectopic pregnancies (2.4%), preeclampsia (21.5%), gestational diabetes (5.7%), pregnancy induced hypertension (24.1%), caesarean section (62.6%) and preterm delivery (43.1%). These reported maternal and fetal complications are significantly higher than the expected frequency in non-kidney transplant recipients. These findings showed that the incidence of adverse pregnancy outcomes, including preeclampsia, is significantly increased in kidney transplant recipients.
Deshpande, et al., reported on all studies between 2000 and 2010 that discussed pregnancy-related outcomes amongst the kidney transplantation population. A total of 50 studies were included in this review, representing 4706 pregnancies and 3570 kidney transplant recipients. The findings of interest were the incidence of preeclampsia (27%), gestational diabetes (8.0%), caesarean section (56.9%) and preterm delivery (45.6%), all significantly higher than the general US population. The data collected also revealed a 54.3% incidence of hypertension amongst the kidney transplant recipients, corroborating the findings of Majak et al., indicating chronic hypertension as a risk factor to not only preeclampsia development but also adverse pregnancy outcomes. This review also detailed that the most prevalently reported prepregnancy factors that may be useful prognostic markers of adverse pregnancy outcomes are hypertension, elevated serum creatinine and proteinuria. The results of this systematic review and meta-analysis provide evidence for the increased obstetrical complications seen in kidney transplant recipients when compared to normal pregnancies.
Critical appraisal findings
The overall findings of each study were similar in nature, detailing the increased incidence in adverse pregnancy outcomes, specifically preeclampsia, in kidney transplant recipients.
Majak, et al., noted no significant difference between prepregnancy proteinuria in those who developed preeclampsia when compared to those who did not. Significant findings were also not established between the time to pregnancy interval of those who developed preeclampsia when compared to those that did not. These findings contradict the current literature which states that pre-pregnancy proteinuria was found to be associated with a higher risk of developing preeclampsia and the ideal interval time to pregnancy is more than 2 years post renal transplant as per the European best practice guidelines to limit pregnancy adverse events such as preeclampsia. This study did not support the other literature discussed in this review. Proteinuria and immunosuppressive medications were not included in Vannevel et al., study. Furthermore, it did not report the transplant to pregnancy interval; hence comparison between time between transplant to pregnancy could not be made.
Tebet, et al., did not include the renal function of patients prior to pregnancy, which affected the final results of this study as determining the cause of the loss in glomerular filtrate rate was unclear whether it is due to preeclampsia or was it the cause to develop preeclampsia. This study also did not mention a vast number of risk factors for preeclampsia, including maternal and transplantation. The second study by Majak et al., did not report pre-pregnancy renal function. You, et al., although discussing maternal and transplantation associated risk factors in the development of preeclampsia there was no statistical significance in the incidence of preeclampsia in patients with chronic hypertension, contradicting the current literature. Hassan et al., did not mention a large proportion of the risk factors associated with preeclampsia development in kidney transplant recipients, including the maternal and transplantation associated factors. Similar limitations were also noted in the study by Kovac et al., who solely mentioned the incidence of maternal and transplantation risk factors but failed to specify the number of patients that developed preeclampsia as a result.
For the two systematic reviews, similar failings to that of the cohort studies were noted. Shah et al., also did not discuss these risk factors and presented with reporting bias due to the different classification of preeclampsia in the various geographical data included in this study. On the other hand, Desphande et al., mentioned numerous risk factors, including hypertension; however, this review did not distinguish between pre-pregnancy hypertension and gestational hypertension, causing difficulty in estimating the incidence of chronic hypertension as a risk factor for solely preeclampsia development [9]. Besides Majak, et al., the remaining literature all provided evidence that agrees with the current literature regarding the increased incidence of preeclampsia in pregnant women post-renal transplant. Additionally, all studies carry implications for clinical practice in proposing potential predictive markers of preeclampsia development and other adverse pregnancy outcomes in renal transplant recipients. Despite Majak et al., lack of supporting evidence, this still has clinical implications as these findings will need to be investigated further [10].
Risk factors related to underlying maternal factors
Maternal age: The mean maternal age of participants in the literature identified in this review ranged from 29 to 32.8 years. The current literature regarding maternal age as a risk factor for preeclampsia determines that women over 35 years of age have a 4.5-fold increased risk of developing preeclampsia when compared to women aged 25-29 years [11]. Maternal age as a risk factor for preeclampsia has been widely supported in the general population as proved by Lamminpaa et al., who conducted a retrospective cohort study aim of this study was to compare the incidence of preeclampsia development in women above the age of 35 and below the age of 35. The findings of this study was that preeclampsia development is more prevalent in women with advanced maternal age [12]. This study was limited primarily to non-renal transplant recipients; however, the studies discussed in this review investigate this hypothesis in renal transplant recipients and support the current literature, with all studies reporting increased rates of preeclampsia development in renal transplant recipients over the age of 35 (Table 1).
| Author | Transplant to Pregnancy Interval (TPI) | Type of donors | Reason for transplantation | Immunosuppression medication used |
|---|---|---|---|---|
| Majak, et al. | <24 months PE: 4 (6%) No PE: 7 (6%) |
GN: 59 (49.6%) Pyelonephritis: 14 (11.8%) DM2: 9 (7.6%) |
PE prednisolone: 63 (97%) Cyclosporine: 42 (65%) Tacrolimus: None Azathioprine: 45 (69%) |
|
| >24 months PE: 61 (94%) No PE: 103 (94%) |
No PE Prednisolone=108 (98%) Cyclosporine=51 (51%) Tacrolimus=0 Azathioprine=87 (79%) |
|||
| Vannevel et al. | PE 75.2 months ± 39.4 No PE 72.7 months ± 49.7 |
Living=13 5/13 had PE Deceased=39 15/39 had PE |
Chronic pyelonephritis n: 15 GN n: 8 |
|
| Tebet et al. | Mean: 5 years Median: 4 SD: 4 |
Deceased n: 23 (53.5%) Living n: 20 (46.5%) |
Glomerulopathy n: 23 (53.5%) Hypertension n: 3 (7.0%) UTI n: 2 (4.5%) Vesicoureteral reflux n: 2 (4.5%) DM n: 1 (2.5%) Unknown n: 12 (28.0%) |
|
| Majak et al. | ||||
| You et al. | <2 years=10 50% had PE >2 years=31 33.3% had PE |
Living: 23 Deceased: 6 | Chronic GN: 12 HTN: 4 DM2: 1 Unknown: 12 |
Cyclosporine 24 (35.3% PE) Tacrolimus 16 (33.3% PE) |
| Hassan et al. | Group A 24 pts>24 months Group B 20 pts<24 months After transplant |
Living: 44 Deceased: 0 |
GN Group A (24 pts)=62.5% Group B (20 pts)=60% Reflux Group A=16.6% Group B=20% Undetermined Group A=20.8% Group B=20% |
|
| Kovac et al. | 95.4% after 24 months 1 was <24 months | Deceased n: 15 Living n: 3 |
GN=8 Reflux Nephropathy=5 APCKD=2 Chronic pyelonephritis=1 Unknown=2 |
Cyclosporine (82%) Tacrolimus (14%) Azathioprine (68%) Methylprednisolone (91%) |
| Shah et al. | <2 years=13% 2-3 years=24% >3 years=23% *% developed preeclampsia |
|||
| Deshpande et al. | Systemic review 3.2 years (3.1-3.3) Meta-analysis occurrence of PE <2 years=39.4% 2-3 years=35.5% 3-4 years=30.1% >4 years=20.6% |
Table 1. Maternal factors as associated risk factors.
Pre-pregnancy renal function: Renal function encompasses numerous measurements, including serum creatinine levels and glomerular filtration rate. In pregnant women with preeclampsia, we would expect the glomerular filtration rate to decrease modestly, a result of the increased afferent arteriolar resistance. However, the findings of this review suggest that these figures are drastically decreased in post renal transplant recipients, with Vannevel et al., noted a significant difference between glomerular filtration rate at delivery and at the time of conception (P=0.03). Serum creatinine levels are also identified as an important predictive marker of preeclampsia development in renal transplant recipients. You et al., provides evidence to support the current literature, noting a 7.7 times increased risk of preeclampsia in patients with a pre-pregnancy serum creatinine of greater than 1 mg/dL. Kidney transplant women with stable allograft function has better pregnancy outcomes than those with underlying decline in renal function. Efforts in determining the ideal time for conception post renal transplant with vigilant monitoring for any deterioration in allograft function and occurrence of preeclampsia during pregnancy is important to reduce the risk of maternal, fetal and allograft complications.
Pre-pregnancy hypertension: Hypertension is a common development in renal transplant recipients prior to pregnancy, with the literature estimating the incidence between 52% and 69%. A vast number of factors play a role in the onset of hypertension in these patients, in addition to exacerbating existing hypertension. These include the baseline allograft function, the type of immunosuppressive medications, the type of donor, obesity, smoking and the presence of a native kidney causing increased renin production.
Hypertension is considered an important risk factor in the diagnostic criteria for preeclampsia; however, the current literature on the topic of pregnancies post renal transplant fails to evaluate hypertension as a significant predictive factor for the development of adverse outcomes, including preeclampsia. Fox et al., noted that hypertensive disorders affect an estimated 10% of all pregnancies and are defined as new onset hypertension after 20 weeks gestation. This definition incorporates preeclampsia; however, pre-existing hypertension can significantly increase the likelihood of the development of hypertensive disorders during pregnancy, especially in post renal transplant patients.
The literature included in this review has predominantly corroborated hypertension as an important prognostic factor in the development of preeclampsia in pregnancy post renal transplantation [13]. These findings are in line with similar research conducted in the general population.
Pre-pregnancy diabetes mellitus: The risk of preeclampsia development is increased two to four-fold among women with either type 1 or type 2 diabetes mellitus. However, the current literature details the significant challenge posed to investigating the correlation between these two diagnoses due to the limited number of pregnant women with pre-existing diabetes and the vast number of difficulties presented in the diagnosis of preeclampsia. In the literature identified in this review, one study discussed the development of preeclampsia in renal transplant recipients with pre-existing diabetes mellitus. Majak et al., recorded preeclampsia in 5 patients (7.7%) with diabetes mellitus diagnosed before pregnancy. These findings represent over a 2-fold increase in the incidence of preeclampsia; however, these results were not significant (P=0.20). The limited data surrounding the incidence of preeclampsia development in renal transplant recipients with prepregnancy diabetes mellitus warrants further studies into this high-risk population to determine the risk associated with adverse pregnancy outcomes.
Pre-pregnancy proteinuria: Combs et al., evaluated the hypothesis that the risk of preeclampsia is significantly increased in diabetic mothers with proteinuria, with the findings of this cohort study in favour of this hypothesis [14]. The results from 311 participants revealed that diabetes mellitus with early-pregnancy and pre-pregnancy proteinuria of 190 mg/day-499 mg/day significantly increased the risk of preeclampsia development. However, the implications of pre-pregnancy proteinuria are not widely studied in renal transplant recipients.
This review aims to provide evidence in minimising this gap in the literature, with three of the included studies discussing the impact of pre-pregnancy proteinuria on the development of preeclampsia in renal transplant recipients. Majak et al., assessed the incidence of preeclampsia in patients with prepregnancy proteinuria, with 3% of participants who developed preeclampsia presenting with pre-pregnancy proteinuria. Although these findings were not significant, the over 3-fold increase in preeclampsia development warrants further investigation. You et al., also noted an increase in preeclampsia development in patients with pre-pregnancy proteinuria, with 17 participants diagnosed with this adverse pregnancy outcome; however, as with Majak et al., these findings were not significant (P>0.05). Kovac et al., on the other hand, demonstrated a significant increase in the incidence of preeclampsia development in those who presented with proteinuria prior to pregnancy, with this retrospective study validating that proteinuria is a risk factors for preeclampsia development after kidney transplantation. Hassan et al., study aim was to compare pregnancy outcomes between differing transplant to pregnancy intervals. Although not directly investigating the implications of pre-pregnancy proteinuria itself, this study noted that proteinuria was significantly increased in those who became pregnant within 24 months of renal transplantation.
Risk factors related underlying renal transplantation
Transplant to pregnancy interval: The ideal period between renal transplantation and pregnancy is a controversial issue. According to the guidelines detailed by the American society of transplantation, the optimal time for conception, post kidney transplant, is between one and two years; however, the European best practice guidelines recommend delaying pregnancy for two years after transplantation. Hassan et al., concluded that, regarding maternal complications, including preeclampsia, the difference between transplantation to pregnancy intervals of less or more than two years was not significant, with most women included in this comparison study becoming pregnant after two years of transplantation. Shah et al., on the other hand, noted that a transplant to pregnancy interval of more than two years increases the risk of preeclampsia development [15]. This was contradicted by Deshpande et al., whom found that a shorter transplant to pregnancy interval, less than two years post transplantation, significantly increased the risk of preeclampsia; however, only three studies included in this metaanalysis evaluated participants with a transplant to pregnancy interval of fewer than two years, giving to an overall limitation of this study.
Type of donors: The type of donor has been identified across several studies as a risk factor to preeclampsia development in renal transplant recipients, with the current literature suggesting that the incidence of preeclampsia is increased amongst living kidney donors. Only five of the nine studies assessed in this review discussed the type of donor used during renal transplantation, whether that be a living donor or cadaver. However, all studies failed to assess the type of donor as a risk factor to preeclampsia development and the significance of these findings, with solely Vannevel et al., reporting the incidence of preeclampsia in both living (38.5%) and deceased (38.5%) donors.
Aetiology of chronic kidney disease: The reason for transplantation was reported in six of the studies evaluated, with the most reported causes being chronic glomerulonephritis, hypertension and pyelonephritis. Despite the different underlying pathologies that resulted in the primary renal transplantation being discussed, the impact that each pathology had on the development of preeclampsia failed to be assessed in any of the identified literature. Moreover, a thorough assessment of the current literature concerning the reason for transplantation as a risk factor to preeclampsia in transplant recipients revealed no conclusive evidence in support of this correlation to diagnosis.
Use of immunosuppression medications
There is a vast amount of literature regarding the use of immunosuppression medications and their impact on preeclampsia development in pregnant women; however, this relationship is not widely assessed in renal transplant recipients. Majak et al., recorded the number of preeclampsia patients taking immunosuppressive medications which are like those without a diagnosis of preeclampsia, suggesting that the use of immunosuppressive medication is not a risk factor to the development of preeclampsia in renal transplant recipients. This study was the only literature in this review that compared the use of immunosuppressive medications between renal transplant recipients who developed preeclampsia. Therefore, further investigations are required to establish if a relationship is present between the use of immunosuppressive medications and the development of preeclampsia in renal transplant recipients.
Aspirin as prophylaxis against preeclampsia
In recent years, aspirin has been approved as both a protective and prophylaxis measure against preeclampsia in the general population. Research has shown that aspirin is safe to use during pregnancy and moderately reduces the relative risk of preeclampsia and other hypertensive associated events. The Collaborative Low-dose Aspirin Study in Pregnancy (CLASP) trial evaluated the administration of low-dose aspirin for the prevention and treatment of preeclampsia. Overall, the CLASP trial provides evidence for the prophylactic and therapeutic administration of aspirin in pregnancy for women at an increased risk of preeclampsia, including women post renal transplantation. This study, in corroboration with the current literature, resulted in the adaption of aspiring administration to a lower dosage in pregnancies of a high risk of preeclampsia development with underlying renal disease.
This review discusses three individual articles that evaluate the use of aspirin during pregnancy post renal transplant; however, all three studies failed to provide sufficient evidence regarding the positive outcomes aspirin may yield. This lack of findings is a result of the small number of participants that were enrolled in each study, an overall limitation of the studies identified. Despite this, although aspirin has not been widely studied in women who have received renal transplantation, it should be strongly considered as a potential preventative treatment for the development of preeclampsia in all renal transplantation pregnancies.
Several risk factors have been identified in the development of preeclampsia in renal transplant recipients, including those related to underlying maternal factors and renal transplantation factors. The underlying maternal factors are most significant in the increased incidence of preeclampsia in this high risk population, maternal age, pre-pregnancy renal function and hypertension being the most prevalent risk factors. Additional factors, such as pre-pregnancy diabetes mellitus and proteinuria, have also been identified as potential risk factors; however, the literature regarding this hypothesis is limited, warranting further studies for validation. Renal transplantation factors also pose an increased risk to preeclampsia, with the transplant to pregnancy interval being the largest determinant to this adverse pregnancy outcome’s development.
Several predominantly maternal factors increase the risk of preeclampsia development in renal transplant recipients, with thorough counselling on these issues given to patients prior to conception crucial in minimising the incidence of adverse pregnancy outcomes.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shamsi HA. "Extended Literature Review of Predicators of Preeclampsia in Pregnant Renal Transplant
Recipients". J Kidney, 2023, 9(2), 1-7.
Received: 15-May-2023, Manuscript No. JOK-23-24155; Editor assigned: 18-May-2023, Pre QC No. JOK-23-24155 (PQ); Reviewed: 01-Jun-2023, QC No. JOK-23-24155; Revised: 01-Sep-2023, Manuscript No. JOK-23-24155 (R); Published: 29-Sep-2023, DOI: 10.35248/2472-1220.23.9.2.14
Copyright: © 2023 Shamsi HA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.