Case Report - (2023) Volume 8, Issue 5
Pemphigus vulgaris is an autoimmune vesiculobullous skin disease. The etiology of this disease remains obscure, although the presence of autoantibodies is consistent with an autoimmune disease (IgG and C3 Complexes). This case report describes the case of a male patient, 59-years-old who complained of numerous flaccid blisters and skin erosion accompanied by pain and an unpleasant odor on the whole of his body that appeared six months ago. His skin disease has been treated using several topical medicines (steroid found), painkiller (acetaminophen), some short-course antibiotics, and no ingested traditional or herbal medicine, but the body didn't heal. Healthcare needs to do a complete assessment based on the patient's signs and symptoms. However, with proper examination and medicine, pemphigus vulgaris can be challenging to treat.
Pemphigus vulgaris • Autoimmune disease • Autoantibodies • Flaccid blisters • Healthcare • Ulcer • Case report
Healthcare providers often underdiagnose pemphigus vulgaris because of the variation of the symptoms. Autoimmune vesiculobullous skin disease causes intraepidermal blister formation [1]. The etiology of this disease remains obscure, although the presence of autoantibodies is consistent with an autoimmune disease (IgG and C3 Complexes). The mortality from this disease is 5%-15% in America, with an incidence rate of 0.5-3.2 cases/100.000, and the prognosis is good [2].
This case report describes the case of a male patient, 59-yearsold who complained of numerous flaccid blisters and skin erosion accompanied by pain and an unpleasant odor on the whole of his body that appeared six months ago. The flaccid blister appeared on his trunk and spread all over his body, scalp, extremities, and oral cavity. The blisters were easy to be broken and revealed painful erosion. He had oral mucous lesion months before the blister appeared and difficulty swallowing, but no cough or hoarseness was found. Since being diagnosed with highly susceptive pemphigus vulgaris, his skin disease has been treated using several topical medicines (steroid found), painkiller (acetaminophen), and some short-course antibiotics, and no ingested traditional or herbal medicine. Based on the history and examination, a provisional diagnosis of pemphigus vulgaris was made. However, the differential diagnosis included mucous membrane pemphigoid and pemphigus bullousa, and the patient has no comorbidities.
His general status was good, with blood pressure 120 mm Hg/70 mmHg, heart rate 100x/mins, respiratory rate 20x/mins, and no abnormalities found in internal organs.
From dermatological status at scalp, trunk, and extremities: There were some flaccid blisters based on non-erythematous skin, variation in shape with diameter 3-5 cm, contained with clear fluid, no tendency to form a cluster/group, nikolsky's sign (+), easy to be broken, revealed numerous painful erosions areas that covered by crust, necrotic tissue and pus, mousy odor (+) and nails dystrophies (Figures 1-4).

Figure 1: Multiple skin erosion.
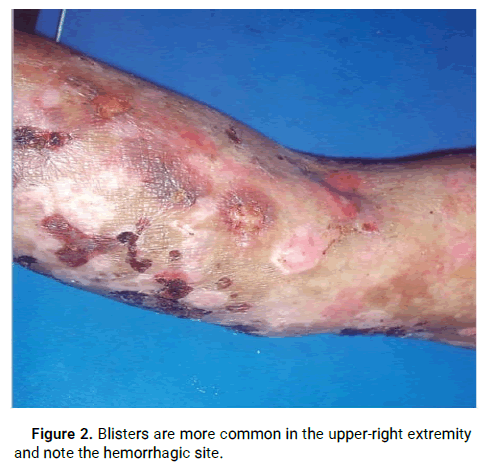
Figure 2: Blisters are more common in the upper-right extremity and note the hemorrhagic site.
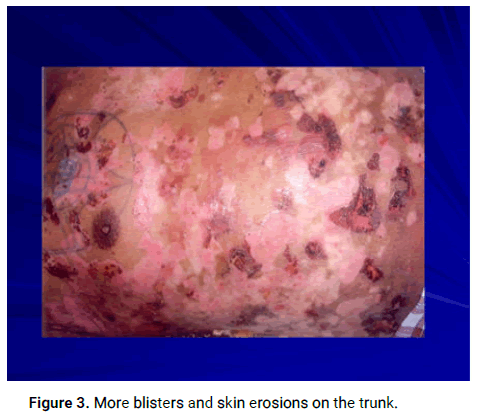
Figure 3: More blisters and skin erosions on the trunk.
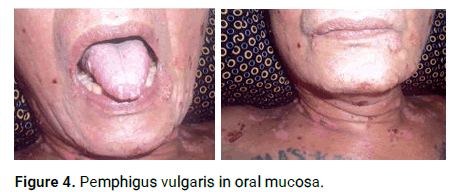
Figure 4: Pemphigus vulgaris in oral mucosa.
From laboratory results, complete blood sample and clinical biochemist marker measured with result Hb 12,1 mg/dl, leucocyte 13.600/Ul, ESR 37 mm/hr, 66 mm/hr, diff. count 75.1/18.2/6.7/6.7/1.6/0.6 ,a lbumine 2.4 g/dL, SGOT 33 u/L, SGPT 24 u/L, ureum 11 mg/Dl, SC 1.0 mg/Dl, RBS 142 mg/d, natrium 13, 9 mmol/L, Kalium 4.1 mmol/L.
From urinalysis were found, leucocyte 0-1 cell, epithelial 0-1 cell, blood, glucose, ketone, protein bilirubin, and urobilinogen were not found or were in the normal range. The gram-smear examination found no coccus but many PMNs in the microscopic sample. And from the biopsy (histopathologic sample) result, was found a skin tissue covered by the epidermis, subepidermal blister (+), acantholytic cell (-), eosinophil (+).
Although with proper examination and proper medicine, pemphigus vulgaris can be challenging to treat because the recurrence rate is still higher in both genders. The infection rate is higher in a tropical country like Indonesia than in a non-tropical country. And the loss of moisture in the skin may worsen the disease. Pemphigus can lead to infection, malnutrition, medication side effects, and death [3]. HLA class II alleles are associated with pemphigus vulgaris in Ashkenazi Jews and non-Jewish patients. Pemphigus vulgaris is caused by autoantibodies targeting keratinocyte proteins, leading to acantholysis and loss of adhesion [4]. Systemic corticosteroids are the first-line treatment of mild pemphigus Vulgaris, which can take several weeks to achieve a response.
Azathioprine is a purine analog that inhibits purine synthesis and should be discontinued if no improvements are seen within three months [5,6]. Rituximab stops B lymphocytes from maturing into autoantibody-producing plasma cells.
In this case, we are using a combination of general topical and systemic medicine. A 20% intravenous albumin was given during hospitalized period (10 days), and IV normal saline infusion was to achieve the target fluid balance. An antibiotic was given orally, Tetracyclin 500 mg t.i.d, systemic corticosteroid was given orally using Prednisone tablet 20 mg t.i.d, and for local mucosal treatment using Borax-Gliserin ointment and roborant tablet t.i.d. Nutrition education also performed to the patient and family for achieving a good level of proteins and calories. This diet is maintained as long as the lesion is still wet. After ten days of hospitalization, the patient was discharged with a systemic treatment change from antibiotic to autoimmune medicine, using azatiophrine 50 mg b.i.d, a long-systemic corticosteroid using Prednisone (fixed dose). A combination of topical ointment (Borax-Gliserin for mucosal, natrium fusidate for the skin), the patient also suggested maintaining adequate dressing using normal saline (moist dressing) and high caloriesprotein diet. The result was good with three months of therapeutic time (Figure 5).

Figure 5: Before and after 3 months of treatment.
Healthcare providers need to do a complete assessment based on the patient's signs and symptoms to ensure early diagnosis and treatment, which determines the disease's prognosis and cause.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Cahayani AC, et al. "Challenges in Management of a Rare Disease Pemphigus Vulgaris: Tailor Made Approach to Improve the Outcome: A Case Report". Dermatol Case Rep, 2023, 8(5), 1-2.
Received: 19-Jun-2023, Manuscript No. DMCR-23-25195; Editor assigned: 21-Jun-2023, Pre QC No. DMCR-23-25195 (PQ); Reviewed: 05-Jul-2023, QC No. DMCR-23-25195; Revised: 28-Aug-2023, Manuscript No. DMCR-23-25195 (R); Published: 05-Sep-2023, DOI: 10.35248/2684-124X.23.8(5).013
Copyright: © 2023 Cahayani AC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.