Research Article - (2024) Volume 15, Issue 3
Background: Hepatitis C Virus (HCV) infection is a globally prevalent pathology and one of the leading cause of death and morbidity. Cholelithiasis is formation of stones inside the gall bladder lumen. This disorder is a major public health problem and increases in incidence in both genders and all races with aging. There are multiple factors that may contribute to the development of gallstones in patients with chronic HCV related liver disease.
Objective: To determine the frequency of cholelithiasis in patients with chronic hepatitis C and compare the frequency of cholelithiasis among cirrhotic and non-cirrhotic hepatitis C.
Study design: Cross sectional study.
Setting: Department of diagnostic radiology, PAEC general hospital H-11/4 Islamabad.
Duration: 6 months i.e., 30-1-2019 to 30-7-2019.
Data collection procedure: Patients fulfilled the study inclusion criteria were selected from OPD. The patients were divided into two groups. Cirrhotic and non-cirrhotic the control group. All the patients were assigned to ultrasound scanning. After that the frequency of cholelithiasis in group A and the control group is seen. Data was entered and analyzed using SPSS software version 17.0.
Results: The mean age of patients was 45.54 ± 14.38 years. There were 66 (47.1%) males and 74 (52.9%) females. In 70 (50%) patients who had cirrhotic HCV while 70 (50%) had non-cirrhotic HCV. In this study, 59 (52.1%) patients had cholelithiasis while 81 (57.9%) did not had cholelithiasis. In cirrhotic HCV patients, 42 (60%) patients had cholelithiasis while 28 (40%) did not had cholelithiasis. In non-cirrhotic HCV patients, 17 (24.3%) patients had cholelithiasis while 53 (75.7%) did not had cholelithiasis. The difference between both groups was significant (p<0.05).
Conclusion: Thus the frequency of cholelithiasis is high in HCV patients and significantly associated with HCV along with presence of cirrhosis.
Cirrhosis; Cholelithiasis; Hepatitis C virus; Gall stone disease
Hepatitis C Virus infection is a globally prevalent pathology and one of the leading cause of death and morbidity. It is the commonest cause of cirrhosis in Pakistan. About 7 million people in Pakistan are suffering from chronic viral hepatitis which can lead to liver cirrhosis. Cholelithiasis is formation of stones inside the gall bladder lumen. This disorder is a major public health problem and increases in incidence in both genders and all races with aging. The risk factors for cholelithiasis include female gender, metabolic syndrome, hyperlipidemia, obesity, cirrhosis, diabetes mellitus and increased estrogen levels.
Historical background of HCV
Most patients with acute and chronic infection are asymptomatic. Patients and healthcare providers may detect no indications of these conditions for long periods; however, chronic HCV infection and chronic active hepatitis are slowly progressive diseases and result in severe morbidity in 20%-30% of infected persons [1]. A HCV is a worldwide problem. The HCV is a major cause of both acute and chronic hepatitis. The World Health Organization estimates about 71 million people globally have chronic HCV, with approximately 399,000 dying from this infection as primarily due to cirrhosis and hepatocellular carcinoma.
The prevalence of HCV infection varies throughout the world. For example, Frank, et al. reported in 2000 that Egypt had the highest number of reported infections, largely attributed to the use of contaminated parenteral antischistosomal therapy. This led to a mean prevalence of 22% of HCV antibodies in persons living in Egypt.
Genotypes
HCV genomic analysis by means of an arduous gene sequencing of many viruses has led to the division of HCV into six genotypes based on homology. Numerous subtypes have also been identified. Arabic numerals denote the genotype and lower-case letters denote the subtypes for lesser homology within each genotype.
Molecular differences between genotypes are relatively large, and they have a difference of at least 30% at the nucleotide level. The major HCV genotype worldwide is genotype 1, which accounts for 40%-80% of all isolates. Genotype 1 also may be associated with more severe liver disease and a higher risk of hepatocellular carcinoma. Genotypes 1a and 1b are prevalent in the United States, whereas in other countries, genotype 1a is less frequent [2]. Genotype details are as follows:
• Genotype 1a occurs in 50%-60% of patients in the
United States.
• Genotype 1b occurs in 15%-20% of patients in the
United States; this type is most prevalent in Europe, Turkey, and
Japan.
• Genotype 1c occurs in less than 1% of patients in the
United States.
• Genotypes 2a, 2b, and 2c occur in 10%-15% of patients in
the United States; these subtypes are widely distributed and
are most responsive to medication.
• Genotypes 3a and 3b occur in 4%-6% of patients in
the United States; these subtypes are most prevalent
in India, Pakistan, Thailand, Australia, and Scotland.
• Genotype 4 occurs in less than 5% of patients in the
United States; it is most prevalent in the Middle East and Africa.
• Genotype 5 occurs in less than 5% of patients in the
United States; it is most prevalent in South Africa.
• Genotype 6 occurs in less than 5% of patients in the
United States; it is most prevalent in Southeast Asia,
particularly Hong Kong and Macao.
Historical background of cirrhosis
Cirrhosis is a condition in which the liver does not function properly due to long-term damage. This damage is characterized by the replacement of normal liver tissue by scar tissue. Typically, the disease develops slowly over months or years [3]. Early on, there are often no symptoms. As the disease worsens, a person may become tired, weak, itchy have swelling in the lower legs, develop yellow skin, bruise easily, have fluid build-up in the abdomen, or develop spider-like blood vessels on the skin.
Epidemiology
Chronic liver disease and cirrhosis result in about 35,000 deaths each year in the United States. Cirrhosis is the ninth leading cause of death in the United States and is responsible for 1.2% of all US deaths. Many patients die from the disease in their fifth or sixth decade of life.
Each year, 2000 additional deaths are attributed to fulminant hepatic failure. It may be caused viral hepatitis (eg, hepatitis A and B), drugs (eg, acetaminophen), toxins (eg, Amanita phalloides, the yellow death-cap mushroom), autoimmune hepatitis, Wilson disease, or a variety of less common etiologies. Cryptogenic causes are responsible for one third of fulminant cases [4]. Patients with the syndrome of fulminant hepatic failure have a 50%-80% mortality rate unless they are salvaged by liver transplantation. Worldwide, cirrhosis is the 14th most common cause of death, but in Europe, it is the 4th most common cause of death.
Pathophysiology
The liver plays a vital role in synthesis of proteins, detoxification, and storage. In addition, it participates in the metabolism of lipids and carbohydrates. Cirrhosis is often preceded by hepatitis and fatty liver, independent of the cause. If the cause is removed at this stage, the changes are fully reversible. The pathological hallmark of cirrhosis is the development of scar tissue that replaces normal parenchyma. This scar tissue blocks the portal flow of blood through the organ, raising the blood pressure and disturbing normal function. Recent research shows the pivotal role of the stellate cell, a cell type that normally stores vitamin A, in the development of cirrhosis. Damage to the hepatic parenchyma leads to activation of stellate cells, which increases fibrosis and obstructs hepatic blood flow.
Causes
Alcoholic liver disease once was considered to be the predominant source of cirrhosis in the United States, but HCV has emerged as the nation's leading cause of chronic hepatitis and cirrhosis.
Many cases of cryptogenic cirrhosis appear to have resulted from Nonalcoholic Fatty Liver Disease (NAFLD). When cases of cryptogenic cirrhosis are reviewed, many patients have 1 or more of the classic risk factors for NAFLD: Obesity, diabetes, and hypertriglyceridemia. It is postulated that steatosis may regress in some patients as hepatic fibrosis progresses, making the histologic diagnosis of NAFLD difficult. Flavinoids have been reported to have positive effects on key pathophysiologic pathways in NAFLD (eg, lipid metabolism, insulin resistance, inflammation, oxidative stress) and may hold future potential for inclusion in NAFLD treatment.
Clinical presentation
Acute HCV infection becomes chronic in 70% of patients, which represents a high rate of chronicity for a viral infection. Most patients with chronic HCV are asymptomatic or may have nonspecific symptoms such as fatigue or malaise in the absence of hepatic synthetic dysfunction [5]. Patients with decompensated cirrhosis from HCV infection frequently have symptoms typically observed in other patients with decompensated liver disease, such as sleep inversion and pruritus.
Symptoms characteristic of complications from advanced or decompensated liver disease are related to synthetic dysfunction and portal hypertension. These include mental status changes (hepatic encephalopathy), ankle edema and abdominal distention (ascites), and hematemesis or melena (variceal bleeding).
Physical examination
Most patients with HCV infection do not have abnormal physical examination findings until they develop portal hypertension or decompensated liver disease. One exception is patients with extrahepatic manifestations of HCV infection, such as porphyria cutanea tarda or necrotizing vasculitis [6]. Signs in patients with decompensated liver disease include the following:
• Hand signs: Palmar erythema, dupuytren contracture, asterixis,
leukonychia, clubbing
• Head signs: ICTERIC sclera, temporal muscle wasting, enlarged
parotid, cyanosis
• Fetor hepaticus
• Gynecomastia, small testes
• Abdominal signs: Paraumbilical hernia, ascites, caput medusae,
hepatosplenomegaly, abdominal bruit
• Ankle edema
• Scant body hair
• Skin signs: Spider nevi, petechiae, excoriations due to pruritus
Approximately 10%-15% of affected patients have symptoms/signs such as weakness, arthralgias, and purpura; these are often related to vasculitis. The precise pathogenesis of these extrahepatic complications has not been determined, although most are the clinical expression of autoimmune phenomena.
Diagnosis
The gold standard for diagnosis of cirrhosis is a liver biopsy, through a percutaneous, transjugular, laparoscopic, or fine-needle approach. A biopsy is not necessary if the clinical, laboratory, and radiologic data suggests cirrhosis. Furthermore, there is a small but significant risk of complications from liver biopsy, and cirrhosis itself predisposes for complications caused by liver biopsy. The best predictors of cirrhosis are ascites, platelet count <160,000/ mm3, spider angiomata and a Bonacini cirrhosis discriminant score greater than.
Endoscopy
Gastroscopy (endoscopic examination of the esophagus, stomach, and duodenum) is performed in patients with established cirrhosis to exclude the possibility of esophageal varices. If these are found, prophylactic local therapy may be applied (sclerotherapy or banding) and beta blocker treatment may be commenced. Rarely are diseases of the bile ducts, such as primary sclerosing cholangitis, causes of cirrhosis. Imaging of the bile ducts, biliary tract and pancreas may aid in the diagnosis.
Pathology
Macroscopically, the liver is initially enlarged, but with the progression of the disease, it becomes smaller. Its surface is irregular, the consistency is firm, and the color is often yellow (if associated with steatosis). Depending on the size of the nodules, there are three macroscopic types: Micronodular, macronodular, and mixed cirrhosis.
Treatment
Patients with acute HCV infection appear to have an excellent chance of responding to 6 months of standard therapy With Interferon (IFN) [7]. Because spontaneous resolution is common, no definitive timing of therapy initiation can be recommended; however, waiting 2-4 months after the onset of illness seems reasonable.
Treatment for chronic HCV is based on guidelines from the infectious diseases society of America and the American associations for the study of liver diseases, in collaboration with the international antiviral society-USA.
A further criterion is liver biopsy findings consistent with a diagnosis of chronic hepatitis. However, a pretreatment liver biopsy is not mandatory. It may be helpful in certain situations, such as in patients with normal transaminase levels, particularly those with a history of alcohol dependence, in whom little correlation may exist between liver enzyme levels and histologic findings. Patients with normal liver enzyme levels and minimal histologic damage noted on liver biopsy may elect to defer treatment until more effective and less toxic medications become available, whereas patients with more advanced liver injury may prefer to initiate treatment sooner [8]. Patients should be informed that the treatment of HCV infection in the setting of normal liver enzyme levels remains controversial.
IFN and PEG-IFN
The 2 most frequently used recombinant IFN preparations in clinical trials have been IFN alfa-2b (Intron-A) and IFN alfa-2a (Roferon-A), which differ from each other by only a single amino acid residue. IFN alfacon-1 (Infergen), or consensus IFN, is a genetically engineered compound synthesized by combining the most common amino acid sequences from all 12 naturally occurring IFNs. Roferon-A was discontinued from the market in 2007 and Infergen was discontinued from the market in 2013.
PEG-IFN monotherapy
Several reports have documented improved sustained virologic response with PEG-IFN monotherapy. In a randomized study of patients with chronic HCV, Zeuzem, et al., found that PEG-IFN alfa-2a at 180 mcg subcutaneously administered once per week was associated with a higher rate of virologic response than IFN alfa-2a at 6 million U subcutaneously administered 3 times per week for 12 weeks followed by 3 million U 3 times per week for 36 weeks [9]. Findings were 69% versus 28% at week 48 of therapy and 39% versus 19% at week 72 of therapy.
IFNs and ribavirin
A major advance in the treatment of chronic HCV was the addition of the oral nucleoside analogue ribavirin to the IFN regimen. As reported in the landmark 1998 studies by McHutchison, et al. and Poynard, et al., IFN alfa-2b and ribavirin combination therapy for 6-12 months resulted in sustained eradication rates of 30%-40%. However, patients with HCV genotype 1 who were treated for 12 months had a much less favorable response than patients infected with genotypes 2 and 3 who received a 6-month course of therapy.
PEG-IFN therapy with ribavirin
As with IFN alfa, the addition of ribavirin to PEG-IFN heralded a new era in the treatment of chronic HCV. The benefits of combination therapy were documented in 3 landmark trial.
Prognosis
Infection with HCV is self-limited in 15% to 50% of patients. In a review of HCV infection, it was reported that chronic infection developed in 70%-80% of patients. Cirrhosis develops within 20 years of disease onset in 20% of persons with chronic infection.
The onset of chronic HCV infection early in life often leads to less serious consequences. Hepatitis B virus coinfection, iron overload, and alpha 1-antitrypsin deficiency may promote the progression of chronic HCV infection to HCV-related cirrhosis.
Cholelithiasis
Common Bile Duct Stone (CBDS) also known as choledocholithiasis, is the presence of gallstones in the Common Bile Duct (CBD). This condition can cause jaundice and liver cell damage. Treatment is by cholecystectomy and endoscopic retrograde cholangiopancreatography.
This obstruction may lead to jaundice, elevation in alkaline phosphatase, increase in conjugated bilirubin in the blood and increase in cholesterol in the blood [10]. It can also cause acute pancreatitis and ascending cholangitis.
Signs and symptoms of choledocholithiasis
Murphy's sign is commonly negative on physical examination in Cholelithiasis, helping to distinguish it from cholecystitis. Jaundice of the skin or eyes is an important physical finding in biliary obstruction. Jaundice and/or clay-colored stool may raise suspicion of Cholelithiasis or even gallstone pancreatitis [11]. If the above symptoms coincide with fever and chills, the diagnosis of ascending cholangitis may also be considered.
Diagnosis of cholelithiasis
The diagnosis of cholelithiasis is suggested when the liver function blood test shows an elevation in bilirubin and serum transaminases. Other indicators include raised indicators of ampulla of vater (pancreatic duct obstruction) such as lipases and amylases. In prolonged cases the international normalized ratio may change due to a decrease in vitamin K absorption [12]. (It is the decreased bile flow which reduces fat breakdown and therefore absorption of fat soluble vitamins).
Preoperative examinations
Symptoms: Characteristically, the symptom complex of Cholelithiasis consists of right upper abdominal colicky pain, radiating to the right shoulder with intermittent jaundice accompanied by pale stools and dark urine, whereas cutaneous itching is rarely present. In contrast with patients with neoplastic obstruction of the CBD or ampulla of Vater, the gallbladder is usually not distended (Courvoisier’s law). Scholastically, Charcot’s triad (jaundice associated to biliary colic pain and sepsis hyperpyrexia and chills), indicates acute cholangitis; as Cholelithiasis is the most frequent aetiology of such a clinical picture, it should prompt immediate diagnostic confirmation and CBD drainage [13].
Endoscopic examinations
All endoscopic procedures share the pros and cons of peroral endoscopy. Although endoscopically reaching the second duodenum is widely considered to be an easy task for average endoscopists in average patients, some conditions can make this manoeuvre a difficult one. In some cases, the papilla major is difficult to identify and to cannulate, resulting in a challenging situation for the endoscopist (and dangerous for the patient), as it is for example when it is placed in a duodenal diverticulum. Previous surgical procedures on the stomach, such as Roux-en-Y gastric by-pass or gastrectomy with duodenal stump closure and Billroth II reconstruction, are another frequent cause of ERCP failure and complications [14]. In particular, endoscopically reaching the second duodenum is difficult after a Roux-en-Y reconstruction, but also after an “Ω”-shaped anastomosis. In those cases, both CBDS diagnosis and management have to be carried out surgically (open surgery or laparoscopy).
Complications of cholelithiasis
There are complications of gallstones and blocked ducts, some of which may be fatal. These complications include:
• Gallbladder or liver inflammation
• Damage to the gallbladder, bile ducts, or liver
• Bacterial infection
• Gallstone pancreatitis, an inflammation of the
pancreas
• Death.
Management of cholelithiasis
Treatment involves an operation called a choledocholithotomy, which is the removal of the gallstone from the bile duct using ERCP, although surgeons are now increasingly using laparoscopy with cholangiography. In this procedure, tiny incisions are made in the abdomen and then in the cystic duct that connects the gallbladder to the bile duct, and a thin tube is introduced to perform a cholangiography. If stones are identified, the surgeon inserts a tube with an inflatable balloon to widen the duct and the stones are usually removed using either a balloon or tiny basket.
Endoscopic procedures
ERCP+ES: First introduced in 1974, ERCP followed by endoscopic sphincterotomy has become the most widely used method for imaging and treating CBD stones.
The technique consists of the endoscopic identification of the papilla major (Vater papilla), its cannulation in order to perform ERCP and endoscopic sphincterotomy followed by CBDS extraction by Dormia Basket or balloon. Endoscopic sphincterotomy success rate is reported to exceed 90% (Table 1). Although regarded widely as a safe procedure, large series have recently shown 5%-9.8% morbidity and 0.3% to 2.3% mortality, mostly due to postoperative acute pancreatitis, bleeding and perforation; the latter, reported in 0.3%-1% of cases, carries a mortality rate of 16%-18.90% (Figure 1).
| Age (Years) | n | 140 |
| Mean | 45.54 | |
| Standard deviation | 14.38 | |
| Minimum | 20 | |
| Maximum | 70 |
Table 1: Descriptive statistics of age of patients.
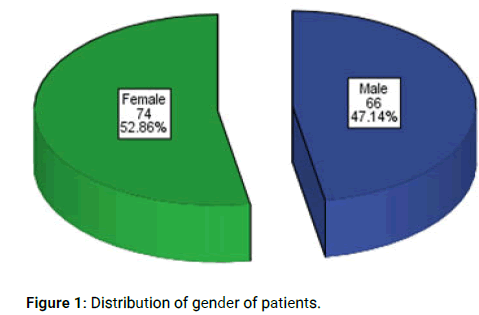
Figure 1: Distribution of gender of patients.
Surgical procedures
Open surgery: Until the late 1980’s, gallstones were treated by open cholecystectomy and CBDS were managed by open CBD exploration and clearance, which was performed by duodenotomy and sphincterotomy or bilio-enteric anastomosis.
Emerging mini-invasive surgical techniques: Recent advances in minimally invasive surgery, including single incision laparoscopy, natural orifice translumenal endoscopic surgery and robotics, to some extent show the possible future of biliary lithiasis management, although lesser dexterity on the part of surgeons, the need for dedicated devices/advanced skills and the intrinsically technical difficulty of CBD exploration limit the diffusion of these approaches to cholecystectomy at the moment (Figures 2 and Table 2).
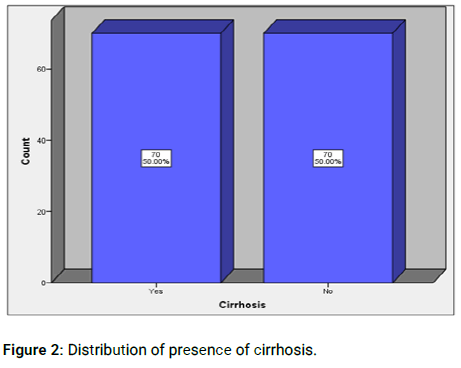
Figure 2: Distribution of presence of cirrhosis.
| Cirrhosis | Total | |||
|---|---|---|---|---|
| Yes | No | |||
| Cholelithiasis | Yes | 42 | 17 | 59 |
| 60.0% | 24.3% | 42.1% | ||
| No | 28 | 53 | 81 | |
| 40% | 75.7% | 57.9% | ||
| Total | 70 | 70 | 140 | |
| 100% | 100% | 100% | ||
Note: Chi-square test=18.309, p-value=0.000
Table 2: Comparison of cholelithiasis in cirrhotic groups.
Lithotripsy
First introduced in 1982, lithotripsy represents the theoretically ideal management of CBDS, as it may enable the clearing of the CBD without any interruption of the CBD wall or sphincterotomy. Although lithotripsy may technically fragmentize gallbladder stones too, it cannot be considered a radical treatment of synchronous cholecysto-choledochal lithiasis, as gallstone etiology is considered as being due to lithogenic bile in the gallbladder (Figure 3).
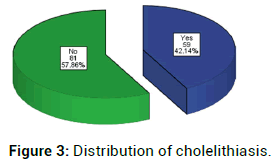
Figure 3: Distribution of cholelithiasis.
HCV is globally distributed and it is estimated that up to 170 million people (3% of the world’s population) are infected worldwide. In Pakistan, about 4.7% of the population is HCV positive. This ranks as the second highest percentage after Egypt (15.5%) (Table 3).
| Age (years) | Cholelithiasis | Cirrhosis | Total | P-value | |
|---|---|---|---|---|---|
| 20-45 | Yes | No | |||
| Yes | 20 | 9 | 29 | 0.014 | |
| 55.6% | 26.5% | 41.4% | |||
| No | 16 | 25 | 41 | ||
| 44.4% | 73.5% | 58.6% | |||
| Total | 36 | 34 | 70 | ||
| 100% | 100% | 100% | |||
| 46-70 | Yes | 22 | 8 | 30 | 0 |
| 64.7% | 22.2% | 42.9% | |||
| No | 12 | 28 | 40 | ||
| 35.3% | 77.8% | 57.1% | |||
| Total | 34 | 36 | 70 | ||
| 100% | 100% | 100% | |||
Table 3: Comparison of cholelithiasis in cirrhotic groups stratified for age.
In our study, the mean age of patients was 45.54 ± 14.38 years. There were 66 (47.1%) males and 74 (52.9%) females. In 70 (50%) patients who had cirrhotic HCV while 70 (50%) had non-cirrhotic HCV. In this study, 59 (52.1%) patients had cholelithiasis. In cirrhotic HCV patients, 42 (60%) patients had cholelithiasis while 28 (40%) did not had cholelithiasis [15]. In non-cirrhotic HCV patients, 17 (24.3%) patients had cholelithiasis while 53 (75.7%) did not had cholelithiasis. The difference between both groups was significant (p<0.05) (Table 4).
The odds of cholelithiasis increased significantly with the severity of liver disease as assessed via elevated serum bilirubin levels and low levels of serum albumin and platelets. In conclusion, chronic HCV infection was strongly associated with cholelithiasis among men but not women in the United States, and cholelithiasis was more common in adults with severe liver disease.
| Gender | Cholelithiasis | Cirrhosis | Total | P-value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Male | Yes | 15 | 13 | 28 | 0.176 |
| 51.7% | 35.1% | 42.4% | |||
| No | 14 | 24 | 38 | ||
| 48.3% | 64.9% | 57.6% | |||
| Total | 29 | 37 | 66 | ||
| 100% | 100% | 100% | |||
| Female | Yes | 27 | 4 | 31 | 0 |
| 65.9% | 12.1% | 41.9% | |||
| No | 14 | 29 | 43 | ||
| 34.1% | 87.9% | 58.1% | |||
| Total | 41 | 33 | 74 | ||
| 100% | 100% | 100% | |||
Table 4: Comparison of cholelithiasis in cirrhotic groups stratified for gender.
Thus the frequency of cholelithiasis is high in HCV patients and significantly associated with HCV along with presence of cirrhosis. Thus we can now recommend the screening of HCV patients for cholelithiasis as presence of cholelithiasis can complicate the condition and quality of life of patients.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Qazi U. "Association between Hepatitic C and Cholelithiasis". J Diabetes Metab, 2024,15(3): 1-6.
Received: 31-Jan-2022, Manuscript No. JDM-23-22318; Editor assigned: 03-Feb-2022, Pre QC No. JDM-23-22318 (PQ); Reviewed: 17-Feb-2022, QC No. JDM-23-22318; Revised: 15-May-2024, Manuscript No. JDM-23-22318 (R); Published: 12-Jun-2024
Copyright: © 2024 Qazi U. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.